 |
Gorgas Case 2011-04 |
 |
|
The following patient was seen in the outpatient department of the Tropical Medicine Institute. We would like to thank Pedro Legua, attending physician, for sharing the case.
History: 30-year-old woman with a 3 day history of chills, fever and the appearance of painful erythematous subcutaneous nodules, 1 to 1.5 cm in diameter, located on the arms, forearms, dorsum of hands and thighs. She reports episodes of similar painful lesions for the last 6 years. Her illness began 6 years ago with the appearance of papular lesions on the forearms and with edema of hands and feet, which progressed to involve the face, ears and thighs. She also had nasal stuffiness, blood tinged nasal secretions, and frank epistaxis. Seen by us in clinic 10 days after starting therapy for this acute episode which had led to some improvement. Epidemiology: Born in the jungle; lives in Lima. Physical Examination (at current clinic visit): Slightly tender erythematous subcutaneous nodules of about 1 cm in diameter on the arms, forearms, dorsum of hands and thighs [Images A, B, C]. Lesions of both earlobes [Image D]. Hypoesthesia on both hands and ulnar aspect of left forearm; hypoesthesia on soles and dorsum of left foot. Corneal anesthesia (no blink reflex). Hypothenar hypotrophy on left palm. Mild decrease in strength in the distribution of the ulnar nerves, more marked on the left hand; patient [on left, Image E] cannot hold paper between 4th and 5th fingers when pulled lightly. Laboratory: No lab performed at this time. 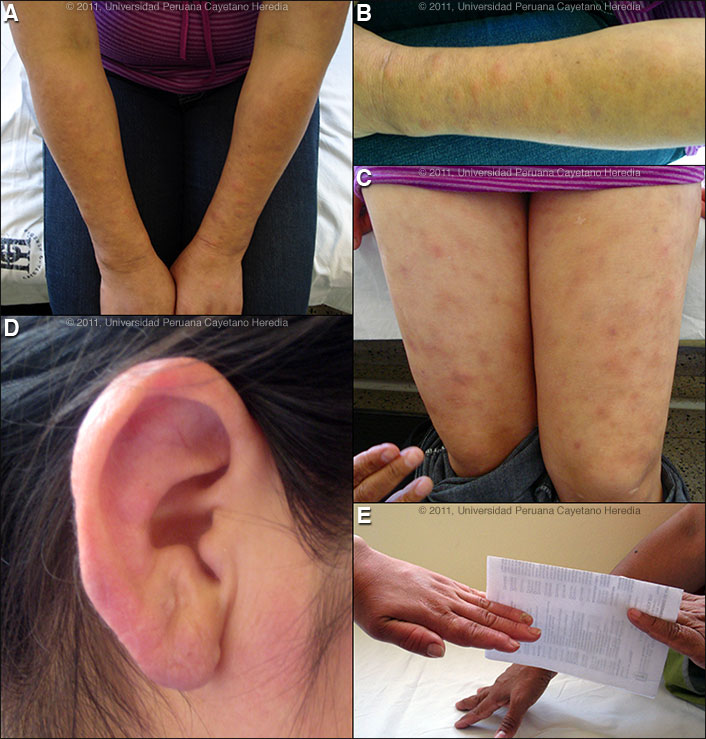
 |
|
Diagnosis: Erythema nodosum leprosum. Lepromatous leprosy (LL).
Discussion: When first seen by us in 2007 she had facial erythema and mild diffuse infiltration of the forehead, malar areas, and earlobes. There were multiple papular lesions as well as subcutaneous nodules on the upper limbs and thighs. At that time there was hypothenar hypotrophy of the left hand and a bilateral mild decrease in strength in the distribution of the ulnar nerves, more marked on the left, and slight thickening of the left ulnar and posterior tybial nerves. Slit skin smears showed 5+ AFB and a skin biopsy showed diffuse lymphohistiocytic inflammatory infiltrate in the dermis, with ill-defined granulomas and with perivascular and periadnexial involvement with abundant acid-fast bacilli on Fite stain. Slit skin smears are performed by making small (5 mm length, 2 mm depth) slits in pinched skin (to avoid bleeding), the edges of which are scraped. The material obtained is smeared on a clean slide and stained for AFB. Generally ear lobes, elbows, and knees are examined. The bacterial index ranges from zero (no bacilli in 100 oil-immersion fields) to 6+ (over 1000 bacilli in one field). She was treated with WHO multi-drug therapy (MDT) for 2 years until 2009. We continue to use 2 years for 4+ or more cases with multibacillary leprosy. The usual and most practical grading system is the WHO classification. For therapeutic purposes, it matters only whether the patient has paucibacillary or multibacillary disease. Where no slit skins smears can be done, paucibacillary leprosy is defined as five or fewer skin lesions; multibacillary cases have six or more lesions. Paucibacillary disease usually presents with small numbers of hypopigmented macules or erythematous plaques with absent or reduced sensation and well-demarcated borders. Multibacillary disease is usually widespread at diagnosis with multiple plaques or infiltrated areas of skin with indistinct borders, non-anesthetic, and papules or nodules. The disease can be classified precisely in the immunologic sense using the traditional Ridley-Jopling classification. This is a spectrum of disease ranging from tuberculoid leprosy (TT) with no AFB in lesions and good cell mediated immunity, to lepromatous leprosy (LL) with many AFB and poor cell-mediated immunity. Leprosy is a disease of peripheral nerves and skin. Leprosy can be diagnosed clinically in any patient with simultaneous skin lesions and sensory loss over the lesions unless there is hyperkeratosis. Type 2 reactions, such as seen here have as the most common presentation erythema nodosum leprosum (ENL). This is a systemic immune mediated disorder, usually with high levels of tissue and circulating TNF-alpha. ENL presents with fever together with many tender erythematous nodules that occurs in up to 50% of lepromatous leprosy cases [Am J Trop Med Hyg. 2006;74(5):868-79] due to their high bacterial loads and in about 10% of those with borderline lepromatous disease. ENL may also produce to varying degrees, neuritis, edema, arthralgias, leukocytosis, uveitis, dactylitis, periostitis, orchitis, lymphadenitis and nephritis. ENL may occur in patients prior to therapy (onset 1.5 years before therapy in this case), during therapy and/or after therapy until the antigen load decreases markedly. ENL may present as repeated acute episodes or may be chronic and ongoing such as in this patient. 
 The standard WHO regimen for paucibacillary disease is 100 mg dapsone a day unsupervised and 600 mg rifampin once per month directly observed for 6 months. For multibacillary disease patients receive 100 mg dapsone and 50 mg clofazimine a day unsupervised and 600 mg rifampin and 300 mg of clofazimine directly observed once per month. A standard WHO multibacillary dose-pack is shown [Image F]; the instructions in English must be clarified for all healthcare staff and patients. WHO now recommends only 1 year of therapy for multibacillary cases [controversy discussed in Lancet. 2004 Apr 10;363(9416):1209-19], but some would treat those with high bacterial indices (4 to 6+) for the previously recommended 2 years due to higher relapse rates as we do here at our institution. A myriad of treatment reactions can occur, the possibility of which should be informed and explained to the patient before starting treatment and a reference text should be consulted prior to initiation of therapy by anyone not familiar with these. ENL can be treated symptomatically if mild or with prednisone or thalidomide if severe. Thalidomide is the drug of choice for severe ENL as in this case and also very effective for neuritis due to type 2 reaction. A dose of 300 to 400 mg daily will usually control the reaction within 48 hours. The dose is then tapered to a maintenance level, which is generally around 100 mg daily and then attempts are made to taper off the drug. This patient has been having recurrent severe ENL beginning 1.5 years prior to her MDT treatment. She has been on thalidomide since 2007 and responds to high doses but every attempt to then taper from 150 mg to 100 mg has led to a recurrent episode of ENL. The current episode was precipitated quickly by the most recent attempt to go from 150 to 100 mg. All women of childbearing age on thalidomide must be on effective contraception up until 6 months after therapy ends. We have treated this episode by increasing the thalidomide back to 300 mg daily for a week but were unsuccessful with a first attempt to go back to 200 mg daily. Uncontrolled ENL can lead to secondary amyloidosis.
|