 |
Gorgas Case 2014-2
Presentation |
 |
| Diagnosis: Envenomation with severe local necrosis due to Bothrops atrox [“jergón” (Perú), common lancehead (USA), fer-de-lance (France)], a common pit viper in nine South American countries. |
|
Severe local swelling, blistering, bruising and necrosis are characteristic of envenomation by vipers and pit vipers but not elapids (cobras, mambas, coral snakes, kraits and others). In addition to the significant local necrosis usually seen, essentially any other organ system may be involved including cardiovascular, renal, hematologic, and CNS. Systemic envenomation (early shock and spontaneous systemic bleeding) when it occurs can be dramatic and potentially life-threatening and more commonly occurs when envenomed by a juvenile B. atrox, whose venom is relatively rich in anti-haemostatic factors and relatively poor in necrotic factors [Toxicon. 2003 Sep 15;42(4):405-11]. The Bothrop’s venom changes in composition as it grows, reflecting its changing prey. In contrast, with elapid envenomation local findings are mostly insignificant and early neurotoxicity often manifest by cranial nerve dysfunction (ptosis, opthalmoplegia) is most prominent. In Perú, as in many countries, many snakebites occur in settings where antivenom may be available in the absence of laboratory facilities. Using the bedside 20-minute whole blood clotting test [demonstrated by Professor Warrell on another patient without coagulopathy; Image D], blood that fails to clot after 20 minutes in an untreated glass tube is a good sign of consumption coagulopathy, which is an indication for antivenom. If the test remains positive (non-clotting) 6 hours after the first dose of antivenom, another dose is needed. Plasma clotting factors or platelets should not be administered until the venom has been neutralized by antivenom or they will merely “fuel the fire” of DIC. Our patient had no evident coagulopathy at initial presentation but was given 2 vials of Instituto Nacional de Salud (Perú) anti-Bothropic polyvalent antivenom intramuscularly due to the severe local necrosis. Intravenous administration is preferable when possible. The antivenom is obtained by immunization of horses with a mixture of the venoms of B. atrox, B. pictus, B. barnetti, B. brazili and B. hyoprora, which is then standardized to have a minimum capacity of 2.5 mg venom B. atrox antivenom neutralized per mL. Pre-treatment with corticosteroid or anti-histamines is still too commonly practiced, but only subcutaneous epinephrine has been proved beneficial and recently steroids have been shown detrimental if given together with epinephrine [PLoS Med. 2011 May;8(5):e1000435]. No early anaphylactoid or pyrogenic reactions complicated our patient’s antivenom therapy even though he was not pre-treated. There is no evidence to support the use of prophylactic antibiotics after snakebite but our patient did receive broad-spectrum coverage on arrival at our hospital emergency room. The risk of envenoming after a Bothrops atrox bite is only about 50%. The practice of giving antivenom to every case of snakebite despite absence of envenoming is widespread. But antivenom is scarce, expensive and dangerous. It should be reserved for patients with systemic or severe, rapidly evolving local envenomation. Anxiety after a bite can result in misleading symptoms including hyperventilation causing acroparaesthesiae, tetany and even syncope. The clinical diagnosis of compartment syndrome of the left arm resulted in urgent fasciotomy where necrosis of the muscle compartments of the arm, forearm and deltoid muscle were found. Continued progression of the necrosis the next day resulted in an above elbow amputation. Two further debridements have yet to control progressive necrosis of the deltoid and further surgical procedures and eventual grafting will be necessary. The pain has resolved. Fatalities due to Bothrops envenomation are common among indigenous peoples in the Amazon basin. The snakes are not aggressive and will only attack if disturbed. Travelers should be educated to be alert when walking in the rainforest. The use of first aid measures such as compression and immobilization in Viperidae envenomation is highly controversial and the aim should be to transport to hospital care quickly. Expedition travelers to remote locations can consider carrying a supply of antivenom but its use does not obviate the need for rapid transport to a medical facility for management of IV fluid administration and support of cardiorespiratory compromise that may ensue. |

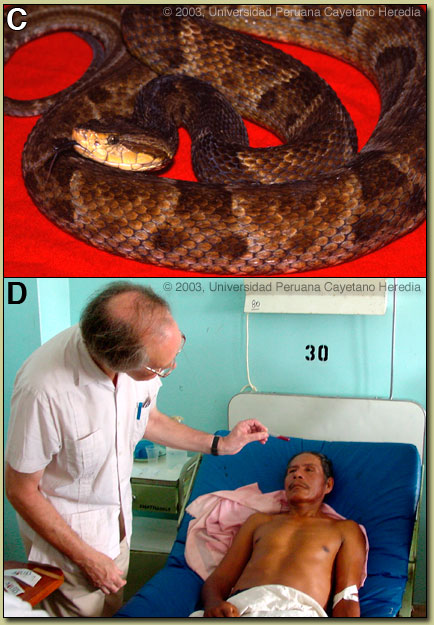 Discussion:Bothrops atrox [shown in Image C] is the most important cause of snakebite deaths and morbidity throughout the whole Amazon region, while other Bothrops species account for most serious snakebites elsewhere in Latin America. Bothrops range from Mexico and The Caribbean to Argentina. They occur in habitats from grasslands to rainforest and some are arboreal. Adult Bothrops atrox range in size from 70 cm to nearly 1.5 m. They possess heat-sensing pits between the eyes and the nostrils. Patients’ descriptions of the snake are often unreliable. Juvenile Bothrops atrox vibrate their white tail-tips when alarmed so sometimes patient will say that they have been bitten by a “cascavel” (literally “rattlesnake”), a name used in northeastern Perú, where there are no rattlesnakes.
Discussion:Bothrops atrox [shown in Image C] is the most important cause of snakebite deaths and morbidity throughout the whole Amazon region, while other Bothrops species account for most serious snakebites elsewhere in Latin America. Bothrops range from Mexico and The Caribbean to Argentina. They occur in habitats from grasslands to rainforest and some are arboreal. Adult Bothrops atrox range in size from 70 cm to nearly 1.5 m. They possess heat-sensing pits between the eyes and the nostrils. Patients’ descriptions of the snake are often unreliable. Juvenile Bothrops atrox vibrate their white tail-tips when alarmed so sometimes patient will say that they have been bitten by a “cascavel” (literally “rattlesnake”), a name used in northeastern Perú, where there are no rattlesnakes.