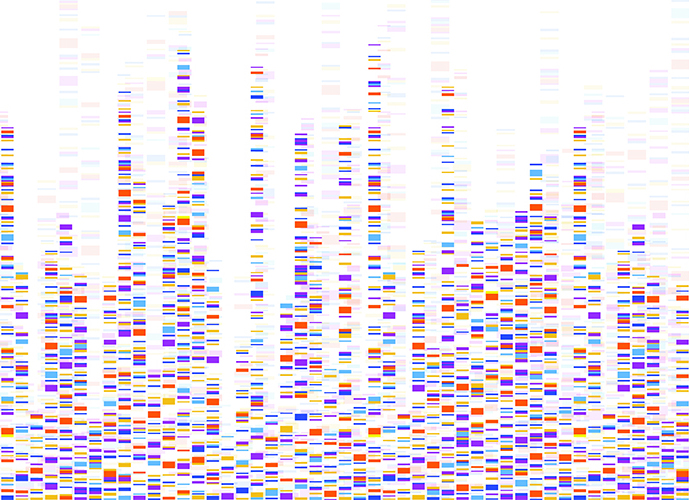
 It is called PAGER-CoV, and it promises to be an important tool in finding therapies for COVID-19. Simply put, PAGER-CoV isa database packed with nearly 12,000 (so far) pieces of genetic information on the SARS-CoV-2 virus, information that researchers and physicians can use to tailor treatments against the disease.
It is called PAGER-CoV, and it promises to be an important tool in finding therapies for COVID-19. Simply put, PAGER-CoV isa database packed with nearly 12,000 (so far) pieces of genetic information on the SARS-CoV-2 virus, information that researchers and physicians can use to tailor treatments against the disease.
PAGER-CoV is an extension of PAGER, a database of gene sets created by Jake Chen, Ph.D., a professor in the Department of Genetics and associate director of the Informatics Institute in the School of Medicine. Chen created PAGER some 10 years ago while he was at Indiana University. As the pandemic spread in early 2020, Chen and his UAB colleagues created a similar system, PAGER-CoV, in response.
The database includes 11,835 PAGs, which stands for pathways, annotated gene lists, and gene signatures:
- Pathways are the roadmap that describes how genes are turned on and off and how they establish connections with each other.
- Annotated gene lists are empirical information that researchers collect from experiments or literature. Gene lists help researchers understand how a certain cell type behaves under different conditions.
- A gene signature is a unique pattern of gene expression within a cell from a single or group of genes, providing information about the activity of those genes in the cell.
 Jake Chen“SARS-CoV-2 is a new virus, and we knew little about its impact on the human body upon viral infection back in the summer of 2020,” Chen says. “The goal here is to gather all this information together in a searchable database so that researchers can gain a better understanding of how the virus’s genes behave or perform under various biophysical conditions, such as severe COVID-19 or long-haul COVID-19 patients.”
Jake Chen“SARS-CoV-2 is a new virus, and we knew little about its impact on the human body upon viral infection back in the summer of 2020,” Chen says. “The goal here is to gather all this information together in a searchable database so that researchers can gain a better understanding of how the virus’s genes behave or perform under various biophysical conditions, such as severe COVID-19 or long-haul COVID-19 patients.”
Chen says SARS-CoV-2 has 15 genes, with scant information on how these genes affect human cells. “We need to understand the differences in people who die from COVID-19 versus the person who only has a mild case of the disease,” he says. “This is a precision medicine approach, employing the database to organize all that we’ve learned about the virus so that the information can be used in an effective way.”
Chen says the downstream effects of coronavirus are not well understood. Better understanding could lead to tailored therapeutics based on gene behavior. “We need to know how the virus proteins are interacting with human cells, and we need to know what we can do about it,” he says. “There is no shortage of possible therapeutics. There is a shortage of regimens that will pair the right therapeutic with the right person. Precision medicine is what this work will help COVID-19 physicians understand.”
Chen and colleagues’ paper on the workings of PAGER-CoV was published in January in Nucleic Acids Research. The team searched the medical literature for all articles dealing with the SARS-CoV-2 virus. They then employed data science tools to do comprehensive data processing and data integration. Supercomputers were used to establish quality measures and develop PAG-to-PAG relationships.
Chen says users can search the database with any human gene or a PAG of interest, drill down to their database entry, and navigate to other related PAGsthrough either shared PAG-to-PAG co-membership relationships or PAG-to-PAG regulatory relationships. To date, there are nearly 20 million PAG-to-PAG relationships stored in the database.
“We intend to provide a resource that researchers doing functional genomic studies of COVID-19 will use,” Chen says. “There is a lot of information here, organized in a way that we hope will spur new insights and lead to meaningful results.” PAGER-CoV will grow as new information is available and added to the database. Chen urges researchers worldwide to make use of the portal and participate in this community-based knowledge curation effort.
PAGER-CoV is freely available to the public without registration or login requirements (http://discovery.informatics.uab.edu/PAGER-CoV/). The data is available for download based on the agreement of citing this work while using the data from the PAGER-CoV website.
Joint first authors of the paper are Zongliang Yue, Ph.D., and Eric Zhang. Additional co-authors are Clark Xu, Sunny Khurana, Nishant Batra, Son Do Hai Dang, and James Cimino, M.D.
PAGER-CoV was developed with support from the UAB Informatics Institute, UAB Academic Enrichment Fund, the UAB Center for Clinical and Translational Science, National Cancer Institute, and the National Center for Advancing Translational Sciences of the National Institutes of Health.
As the COVID-19 vaccine becomes more widely available to the public, immunity monitoring will play an important role in determining whether the vaccine is effective for an individual, and for how long. Benjamin Larimer, Ph.D., has developed a technology with potential use as an in-home antibody test.
Larimer’s diagnostic test is an accurate and reliable method for determining whether individuals are protected against COVID-19. The technology identifies neutralizing antibodies—those that block the virus from infecting cells. Emerging research suggests neutralizing antibodies offer the best protection against the virus.
The most widely used antibody tests today do not specifically identify neutralizing antibodies. Currently, these neutralizing antibodies can only be measured at a high level of accuracy using complicated and time-consuming laboratory tests not available to the general public.
 Benjamin LarimerAccording to Larimer, existing antibody tests use a broad approach to locating antibodies, which attach to very small and distinct pieces of the virus. Current tests can mistake antibodies for other viruses, such as the common cold, for COVID-19 antibodies, leading to possible false-positive results.
Benjamin LarimerAccording to Larimer, existing antibody tests use a broad approach to locating antibodies, which attach to very small and distinct pieces of the virus. Current tests can mistake antibodies for other viruses, such as the common cold, for COVID-19 antibodies, leading to possible false-positive results.
To create the new test, Larimer began breaking down the COVID-19 virus into small pieces to identify the exact locations where antibodies attached to the virus. The results were better than Larimer’s team anticipated, with the test detecting 20 percent more positive cases than the current gold-standard clinical antibody test. The ability to specifically recognize even small amounts of antibodies accurately is an important achievement, according to Larimer.
“The goal of every vaccine is to get the body to produce antibodies, which serve as a first line of defense against the virus,” says Larimer, an assistant professor in the UAB Department of Radiology Division of Advanced Medical Imaging Research. “Tests that specifically detect these antibodies can be used to measure whether a vaccine works, and possibly predict how long its protection will last.”
Immunity to COVID-19 is not anticipated to last forever, and immunity monitoring could continue for several years, even after widespread administration of a vaccine. Antibody testing helps determine vaccine efficacy and should help indicate whether a person is protected against the virus.
Larimer hopes to transition his team’s technology to an inexpensive and easy-to-use test that will provide in-home immunity monitoring for the general public. P3 Diagnostics, LLC, was formed in 2020 by Larimer and co-founders Joe Gay and Chris Paule. The startup serves to foster the business development of technology created under the direction of Larimer and the Larimer Lab. ~Bob Shepard and Briana Bryant