 Unraveling the mystery of long COVID is like solving a complex puzzle. After recovering from an initial COVID-19 infection, some people continue to experience a range of troublesome symptoms that can last for months or even years.
Unraveling the mystery of long COVID is like solving a complex puzzle. After recovering from an initial COVID-19 infection, some people continue to experience a range of troublesome symptoms that can last for months or even years.
These symptoms, like extreme tiredness, brain fog, and difficulty breathing, can be significantly challenging for those affected.
The Heersink School of Medicine communications team sat with Frances Lund, Ph.D., professor in the Department of Microbiology, director of the UAB Immunology Institute, and Nathaniel Erdmann, M.D., Ph.D., associate professor in the Division of Infectious Diseases and hub Principal Investigator for the National Institutes of Health (NIH) Long COVID RECOVER study, to learn more about long-COVID and how UAB is investigating ways to combat it.
Q: What is long COVID, and how does it differ from an acute COVID-19 infection?
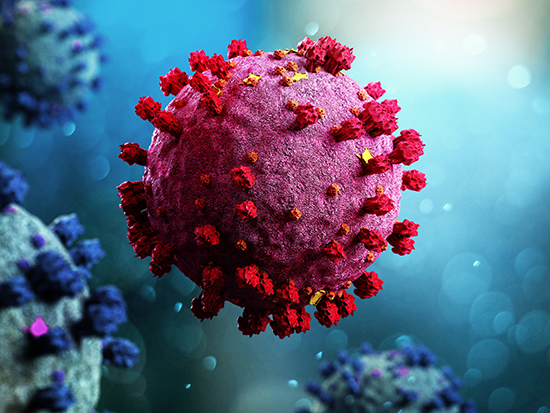
Lund: An acute COVID-19 infection includes the time immediately after infection with SARS-CoV-2. This would include the time that an individual has a detectable virus that could be measured using one of the virus detection kits (typically between five to 15 days post-infection).
It would also include a couple of weeks after the virus is cleared when someone will still be recovering from the infection and may still have a cough or feel fatigued. Individuals with long COVID are identified as continuing to have symptoms that are severe enough to negatively impact their quality of life for months to years after the initial infection.
Q: What are the most common symptoms experienced by individuals with long COVID?
Lund: Common symptoms are varied and can include extreme fatigue, brain fog, loss of smell, gastrointestinal issues, and problems with the heart or lungs.
Q: Are there any specific treatments or strategies available to provide relief for long COVID symptoms? If so, what are they?
Erdmann: The only treatments currently available are medications and interventions re-purposed from other diseases. However, there are a variety of active clinical trials ongoing, some of which UAB is participating in.
I am currently leading two NIH studies at UAB, the first exploring the effectiveness of Paxlovid for those with moderate to severe long COVID, and the second using titrated cardiopulmonary rehabilitation for those with exercise intolerance.
Q: Are there any identifiable trends regarding certain pre-existing conditions that predispose individuals to long COVID?
Lund: It is known that individuals who have experienced more severe symptoms during their acute infection are more prone to developing long COVID. However, it is possible that even patients with relatively mild symptoms can develop long COVID.
Q: How are UAB researchers actively studying long COVID? Are there any specific research projects or initiatives underway?
Lund: Numerous labs across our campus are actively investigating long COVID among patients treated at UAB clinics. One such project, supported by the NIH and directed by me, brings together a diverse team of basic scientists and physician researchers from various departments, including Microbiology and divisions like Infectious Diseases, Preventative Medicine, Clinical Immunology and Rheumatology, and Endocrinology, Diabetes, and Metabolism within the Heersink School of Medicine.
This collaborative effort also involves researchers from UAB’s Schools of Public Health, Health Professions, and Nursing. Our large, multidisciplinary team aims to understand whether certain individuals with existing characteristics of chronic inflammation, like those who are overweight or being treated for type 2 diabetes, are more prone to developing long COVID after being infected with SARS-CoV-2.
Q: What have research efforts revealed thus far?
Lund: Through our investigations, we've identified several systemic metabolites and cytokines significantly elevated in a subset of long COVID patients. Employing advanced techniques such as single-cell RNA sequencing, we're delving into the molecular characteristics of immune cells in subcutaneous fat biopsies collected from long COVID patients.
Our next steps involve determining how specific populations of inflammatory cells in fat tissue relate to systemic inflammatory cytokines or changes in metabolism seen in long COVID patients. By pinpointing these connections, we hope to classify long COVID patients into distinct clinical and biological "endotypes," paving the way for more personalized treatment approaches in the future.
Q: What factors contribute to the complexity of understanding long COVID?
Erdmann: Associations between long COVID and specific populations are complex due to our limited ability to distinguish between different types of long COVID, prompting intensive investigation. Viral factors influencing long COVID include cell types infected by SARS-CoV-2, disease severity, immune response efficiency, virus strain, prior immunity, and treatment.
Institutionally, we're deeply involved in characterizing and managing long COVID. We established a clinical network in late 2020, resulting in over 4,000 referrals. Our team leads UAB's participation in the NIH-sponsored RECOVER study with over 700 participants. Additionally, we're engaged in several clinical trials targeting long COVID alongside multiple research teams exploring its mechanisms.