National Epilepsy Awareness Month is observed throughout the month of November, providing support, awareness, and education to promote understanding and improve the lives of those effected by epilepsy. At UAB, the Epilepsy Center, located within Civitan International Research Center, offers clinical, research, and educational services to patients with epilepsy.
 Zachary Mills, M.D.As one of the largest and most active centers in the country and the only one in Alabama, UAB provides a specialized two-year Epilepsy Fellowship Program that equips trainees with the clinical and surgical skills necessary for high-quality, patient-centered care. Fellows in the program engage in cutting-edge research, making them well-rounded experts in the field of epilepsy care.
Zachary Mills, M.D.As one of the largest and most active centers in the country and the only one in Alabama, UAB provides a specialized two-year Epilepsy Fellowship Program that equips trainees with the clinical and surgical skills necessary for high-quality, patient-centered care. Fellows in the program engage in cutting-edge research, making them well-rounded experts in the field of epilepsy care.
Zachary Mills, M.D., a fellowship alumnus who graduated in June 2024, shares his experiences and insights from his time in the program, highlighting how it shaped his approach to epilepsy care.
Bridging technology and care
Epilepsy is a condition that causes irregular cell activity in the brain, resulting in unusual muscle behavior and sensations, and at times, loss of consciousness. People who have epilepsy may experience difficulties performing daily tasks such as walking and driving. According to the World Health Organization (WHO), around 50 million people worldwide have epilepsy, making it one of the most common neurological diseases globally.
Mills, who found an interest in understanding the inner workings of the brain, was drawn to the field of epilepsy for its unique combination of advanced technology and the opportunity to make a significant impact on patient care.
“Epilepsy has some of the most interesting cases even within an already interesting specialty (neurology)," Mills said. "Testing our theories about localization with EEG, MEG, MRI, PET, etc., is very satisfying, and it is very motivating to be the only specialist who can comprehensively interpret this data and get a patient the appropriate treatment.”
The fellowship program provides training in these advanced diagnostic techniques. Fellows receive extensive hands-on experience with EEG interpretation and long-term monitoring, both of which are key in pinpointing the causes of seizures and developing tailored treatment plans.
He adds, “Treating patients with carefully tailored electrical stimulation, placed into their brain directly into the epileptogenic zone, feels like science fiction. If you like physics and technology like me, you will find no better opportunity to synthesize and apply a vast amount of varied data to a patient in real life like you can in refractory epilepsy workups.”
“On the other hand, observing the human psyche and extremes of mental and physical reactions to the stresses and traumas of life is an eye-opening experience that will hone your own worldview and make you understand yourself and all your future patients better.”
Transforming lives
Many patients who suffer from epilepsy may wait years to receive a clear diagnosis of their symptoms, which may or may not be seizures. Receiving care from an epilepsy specialist and undergoing an Epilepsy Monitoring Unit (EMU) admission can help a patient obtain a definitive diagnosis and receive the right treatment, said Mills.
“I took care of a patient who had full-body convulsions very frequently for almost 10 years, and medications were not helping. She could not keep her job, had a very hard time taking care of her kids and family, and generally felt like her life was completely out of her control.”
“After EMU admission, I could give her a clear diagnosis of Psychogenic Non-Epileptic Spells (PNES) which finally got her the right treatment—cognitive behavioral therapy instead of anti-seizure medications—and gave her a very good chance at controlling her life instead of having it control her.”
Advice for new epilepsy fellows
As Mills reflects on his own journey and the chal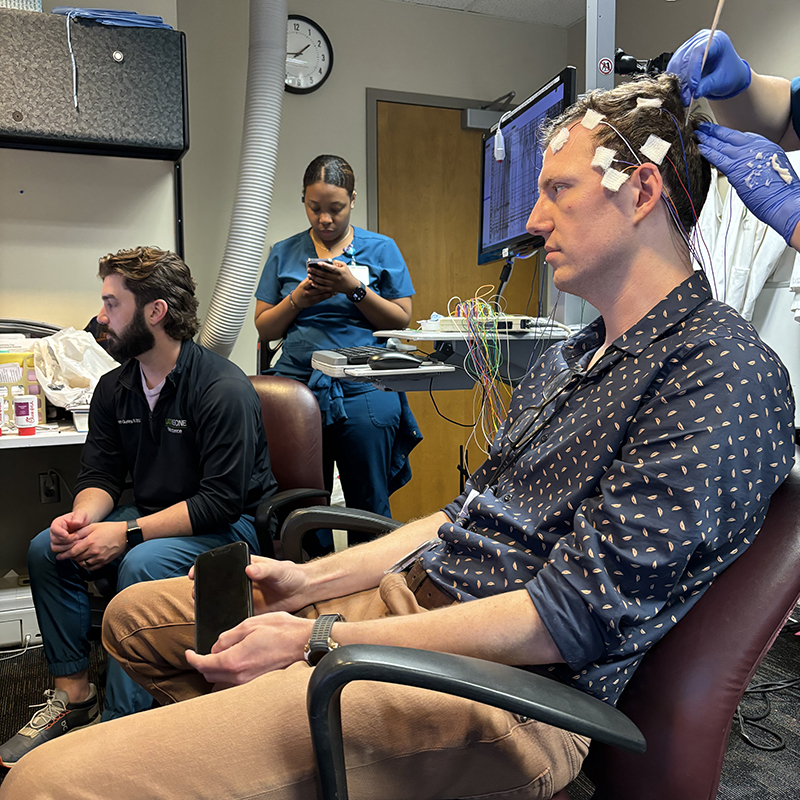 Mills and UAB technicians practice an EEG on him, allowing him to read his own brain activity in real time.lenges that may lie ahead for those entering the field, he offers some advice for future epilepsy specialists.
Mills and UAB technicians practice an EEG on him, allowing him to read his own brain activity in real time.lenges that may lie ahead for those entering the field, he offers some advice for future epilepsy specialists.
“I would advise a new epilepsy fellow to make an effort to create a good collection of epilepsy reference material for themselves to prepare for attending hood,” Mills said.
“Once you graduate, even if you have a great support system at your new job and from your old professors, there is no replacement for being able to personally check on a reliable, accurate, and up-to-date source of epilepsy knowledge. I have several textbooks on both EEG and epilepsy treatment that I frequently reference to answer my day-to-day questions about my new patients.”
The fellowship program also emphasizes the importance of scholarly activity and staying on the cutting edge of research. Fellows are encouraged to participate in ongoing projects or develop their own, with access to a broad range of research opportunities.
Mills’ insights also highlight a deeper truth about the field of epilepsy care: it’s not just about diagnosis and treatment—it’s about truly listening to patients and understanding the unique challenges they face.
As he explains, “These patients will require large amounts of your time to be fully understood on both a medical and psychological level. Being 'the doctor who finally listens' is frequently the only way to finally place these patients on the road to recovery after 5, 10, 15, even 20+ years of misdiagnosis. That is one of the most unique and valuable services we can offer a patient as an epileptologist.”
As we observe National Epilepsy Awareness Month this November, the work of specialists like Mills reminds us of the importance of not only advancing medical knowledge but also offering empathy and unwavering support to those living with epilepsy.
For more information on the Epilepsy Fellowship Program, click here.