Media contact: Yvonne Taunton
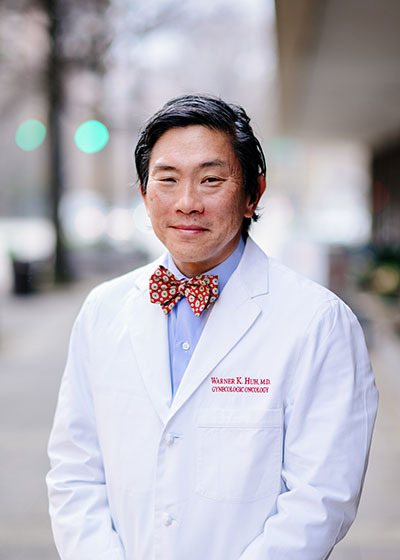 Warner Huh, M.D.
Warner Huh, M.D.
Photography: Andrea MabryAccording to the Centers for Disease Control and Prevention, cervical cancer used to be the leading cause of cancer death for women in the United States. In the past 40 years, the number of cervical cancer cases and the number of deaths have decreased significantly. This decline is based largely on regular Pap tests, which can detect cervical precancer before it turns into cancer. However, 60 percent of women who develop cervical cancer continue to be either unscreened or under-screened.
“Countries that have adopted mass screening have done a significant job in reducing cervical cancer, including the United States,” said Warner K. Huh, M.D., senior scientist at the O’Neal Comprehensive Cancer Center at the University of Alabama at Birmingham.
What is cervical cancer?
Cervical cancer is a type of gynecological cancer that forms in tissues of the cervix, the organ connecting the uterus and vagina. Persistent human papillomavirus is the most significant risk factor for cervical cancer. Acquisition of HPV is closely tied to sexual intercourse and skin-to-skin contact, according to the CDC.
“Most people who get cervical cancer don’t have obvious risk factors,” said Huh, chair of the Department of Obstetrics and Gynecology at the UAB Marnix E. Heersink School of Medicine.“With this type of cancer, what women can control is being screened regularly, getting vaccinated against HPV and seeking medical advice if something doesn’t seem right with their bodies.”
Any woman can be at risk for cervical cancer. Risk tends to increase with age. Lifestyle choices such as chronic smoking can impact one’s risk for developing a gynecologic cancer.
Cervical cancer and impact of COVID-19
COVID-19 has exacerbated the gap between the screened and unscreened. Disruptions of elective health services related to cervical screening, management of abnormal screening test results and treatment of precancers may lead to an increase in cervical cancer incidence.
“Due to the ongoing controversies related to COVID-19 vaccination, we’ve seen a ripple effect on other vaccines — this has had an effect on all preventive vaccinations,” Huh said. “It is a real concern.”
 Learn about the importance of screenings and HPV vaccines to help prevent cervical cancerPap smear vs. HPV tests
Learn about the importance of screenings and HPV vaccines to help prevent cervical cancerPap smear vs. HPV tests
Pap smears have been widely used to detect cervical cancer. The American Cancer Society is highly encouraging HPV tests because they are more sensitive.
According to the CDC, the Pap test looks for precancers, or cell changes on the cervix that might become cervical cancer if they are not treated appropriately, while the HPV test looks for the virus that can cause these cell changes.
“The biggest takeaway for women is to stay mindful of their bodies, report any symptoms that appear even remotely irregular and make sure they have their screenings conducted on a regular basis,” Huh said. “These actions can ultimately save lives.”
Prevention and Detection
Screening is the best way to prevent cervical cancer and ensure timely treatment.
According to Huh, the HPV vaccine is the best protection against cervical cancer. Currently, about 50 percent women in Alabama get vaccinated. Men lag women in vaccination but are strongly advised to also receive the vaccine to protect against cancers caused by HPV. The recommended age for vaccination is 11 to 12 years old, but people can get vaccinated as young as 9 years old or as old as 45.
To schedule an appointment with a UAB Medicine provider, please call 205-934-9999.
