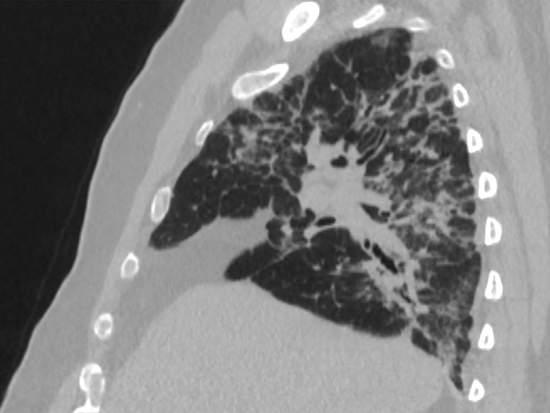
 A Bcl-2 inhibitor that has FDA approval for treatment of several leukemias reversed lung fibrosis in a bleomycin mouse model.Researchers have reversed lung fibrosis in a mouse model of idiopathic pulmonary fibrosis, or IPF, as reported in a study published in the journal Cell Death and Differentiation.
A Bcl-2 inhibitor that has FDA approval for treatment of several leukemias reversed lung fibrosis in a bleomycin mouse model.Researchers have reversed lung fibrosis in a mouse model of idiopathic pulmonary fibrosis, or IPF, as reported in a study published in the journal Cell Death and Differentiation.
Mice were given bleomycin for 12 days to establish lung fibrosis, and then treated daily until 21 days with ABT-199, whose medical form is known as Venetoclax, a medication approved by the United States Food and Drug Administration for use in several forms of leukemia. Control bleomycin mice had lung fibrosis with widespread collagen deposition. The bleomycin mice that received ABT-199 had normal lung architecture at 21 days and no collagen deposition.
These results suggest a novel therapeutic target to reverse fibrotic remodeling in the lungs, says study leader A. Brent Carter, M.D., professor in the Division of Pulmonary, Allergy and Critical Care Medicine in the University of Alabama at Birmingham Department of Medicine. The research was also led by first author Linlin Gu, Ph.D., UAB Department of Medicine.
Pulmonary fibrosis is a chronic disease showing aberrant remodeling of lung tissue. Idiopathic pulmonary fibrosis is the most common form of pulmonary fibrosis and has a high mortality rate within three to five years. Currently approved medications have limited efficacy.
ABT-199 acts by inducing apoptosis, or programmed cell death, in monocyte-derived macrophages in the lung. Macrophages are large white blood cells that engulf and digest anything that does not have the surface proteins of healthy cells. Targets can include cancer cells, microbes and cellular debris.
Previously, fibrosis progression was known to be associated with apoptosis resistance in lung macrophages, though the mechanism of that resistance was poorly understood. Also, existing dogma did not point to macrophages as actors in fibrosis; it instead proposed that increased alveolar epithelial cell injury and apoptosis were the initiating events in lung fibrosis.
Apoptosis is a regulated suicide process for cells that are a threat to the organism or are no longer needed. Mitochondria, the organelles that are the powerhouses of the cell, play a key role in the intrinsic pathway of apoptosis. Carter, Gu and UAB colleagues — seeking to better understand the mechanism of how lung macrophages become apoptotic resistant — soon learned that the mitochondria also play a key role in apoptosis resistance.
Using lung lavage, they isolated macrophages from people with IPF. They found a marked increase in the macrophage mitochondrial protein Bcl-2 — a regulator of apoptosis — as compared to lung macrophages from people without IPF. Mitochondrial Bcl-2 was also elevated in lung macrophages from bleomycin-exposed mice that have lung fibrosis.
Besides increased Bcl-2 in the mitochondria of lung macrophages from bleomycin mice, Carter and colleagues also found two proteins — MCU and Cpt1a — showed a similar increase in expression. The MCU protein is a channel to bring calcium into the mitochondria, and Cpt1a is an enzyme in mitochondria that is the rate-limiting step for the fatty acid beta-oxidation energy pathway. MCU was previously known to regulate metabolic reprogramming of lung macrophages to fatty acid oxidation, as well as act in the progression of lung fibrosis and apoptosis resistance.
The researchers found that Bcl-2 was regulated by MCU, and that silencing MCU caused a significant decrease for Bcl-2 in the mitochondria of lung macrophages. They found that MCU modulated the binding of Cpt1a to a particular domain of Bcl-2, which anchored Bcl-2 in the mitochondria to attenuate apoptosis. This interaction was dependent on Cpt1a activity.
 Brent Carter, M.D.
Brent Carter, M.D.
(Photography: Steve Wood)Looking again at lung macrophages from people with IPF, they found a direct correlation between the levels of Cpt1a and Bcl-2; the amounts in macrophages from different individuals varied in tandem.
Importantly, Carter and colleagues found that mice with a conditional deletion of Bcl-2 in lung macrophages were protected from pulmonary fibrosis in the bleomycin model, and they were also protected from asbestos-induced lung fibrosis. These conditional deletion results set the stage for the experiments showing that the Bcl-2 inhibitor ABT-199 was able to reverse fibrosis in the mouse bleomycin model. Furthermore, ABT-199 completely blocked the Cpt1a-Bcl-2 interaction. In additional genetic evidence, fibrosis was also reversed by the conditional deletion of Bcl-2 in mice with established fibrosis.
“Taken together, these observations suggest that fatty acid oxidation provokes apoptosis resistance through the stabilization of Bcl-2 in the mitochondria by binding to Cpt1a,” Carter said. “Moreover, these data demonstrate that monocyte-derived macrophages are required for fibrosis progression, and they suggest a novel therapeutic target to prevent progressive aberrant fibrotic remodeling.”
Co-authors with Carter and Gu for the study, “Targeting Cpt1a-Bcl-2 interaction modulates apoptosis resistance and fibrotic remodeling,” are Ranu Surolia, Jennifer L. Larson-Casey, Chao He, Dana Davis, Jungsoon Kang and Veena B. Antony, UAB Department of Medicine’s Division of Pulmonary, Allergy and Critical Care Medicine.
Support came from National Institutes of Health grants ES015981-13 and ES027723, Department of Veterans Affairs Merit Review CX001715-01, and Pulmonary Fibrosis Foundation grant 2019650.
At UAB, Carter holds the Department of Medicine Endowed Professorship in Lung Biology.