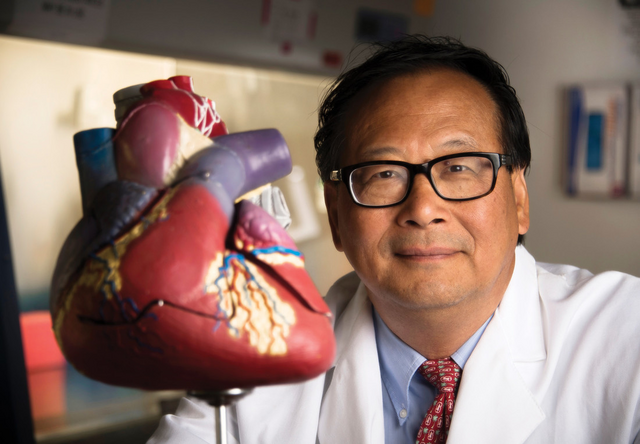
 Jianyi “Jay” Zhang, M.D., Ph.D.,Severe heart attacks often progress to end-stage heart failure because the dearth of heart muscle cells diminishes pumping power of the heart’s left ventricle. The damaged heart, unable to repair itself, deteriorates and enlarges into congestive heart failure.
Jianyi “Jay” Zhang, M.D., Ph.D.,Severe heart attacks often progress to end-stage heart failure because the dearth of heart muscle cells diminishes pumping power of the heart’s left ventricle. The damaged heart, unable to repair itself, deteriorates and enlarges into congestive heart failure.
The problem is that mammalian heart muscle cells, known as cardiomyocytes, lose their ability to proliferate shortly after birth. Researchers have long sought to induce these cells to start dividing again after a heart attack. However, continuous proliferation of cardiomyocytes risks the danger of deadly heart arrhythmias.
Now University of Alabama at Birmingham researchers have found a way to thread this needle. For the first time, they demonstrate a modified messenger RNA that: 1) is exceptionally specific to cardiomyocytes, but no other cell type; and 2) transiently induces the generation of new cardiomyocyte cells, but only for less than four weeks. In mouse and pig models, this treatment significantly improved recovery from acute heart attacks — as measured by prominent reduction of the area of dead heart tissue, known as the infarct, and improved left ventricle contractile function — all without increasing the risk of arrhythmias.
The research, led by Jianyi “Jay” Zhang, M.D., Ph.D., and Lior Zangi, Ph.D., is published in the journal Circulation Research. Zhang is chair of the UAB Department of Biomedical Engineering, and Zangi is an associate professor of medicine at the Icahn School of Medicine at Mount Sinai, New York, New York.
The transient, cardiomyocyte-specific generation of new cardiomyocyte cells at the infarct scar was driven by a cardiomyocyte-specific modified mRNA translation system — which the UAB researchers call “cardiomyocyte SMRTs.” This system, developed by Zhang and colleagues, can be used to upregulate the expression of a gene of interest exclusively in cardiomyocytes. Modifying the mRNA enables a cell to read the mRNA to make protein; such modifications were the breakthrough that made the COVID-19 RNA vaccines possible.
The SMRTs has two distinct mRNAs — one for the protein CCND2 that will activate the cell cycle and allow generation of new cells. To make the SMRTs specific for cardiomyocytes, the SMRT also has the mRNA for L7Ae from an Archaea microorganism. In a cell, the L7Ae mRNA creates L7Ae protein, and that L7Ae protein binds tightly to a kink-turn structure engineered into the leading sequences of the CCND2 mRNA. This binding prevents the CCND2 mRNA from entering ribosomes, so no CCND2 protein is made.
The trick for specific CCND2 translation in heart muscle cells is that the L7Ae mRNA has been engineered to have recognition elements for the cardiomyocyte-specific microRNAs miR-1 and miR-208. Those microRNAs recognize and cleave L7Ae mRNA in cardiomyocytes, but not other cell types. Once the shackles of the L7Ae protein have been removed, the CCND2 mRNA is free to make CCND2 protein to activate the cardiomyocyte cell cycle.
 The modified mRNA — delivered after experimental heart attacks — transiently allows heart muscle cells to proliferate, leading to reduced infarct size and improved heart performance compared to untreated animals.The results of the Circulation Research study are an encouraging step forward for potential treatment of heart attacks, especially in the work done with the more clinically relevant large-animal model. Introduction of the SMRTs alleviated the wall stress burden that follows a heart attack by promoting the generation of new cardiomyocytes and by improving the survival of preexisting cardiomyocytes. This resulted in the decrease of left ventricle infarct size, improvement of left ventricle dilatation and wall stresses, and decrease of left ventricle hypertrophy.
The modified mRNA — delivered after experimental heart attacks — transiently allows heart muscle cells to proliferate, leading to reduced infarct size and improved heart performance compared to untreated animals.The results of the Circulation Research study are an encouraging step forward for potential treatment of heart attacks, especially in the work done with the more clinically relevant large-animal model. Introduction of the SMRTs alleviated the wall stress burden that follows a heart attack by promoting the generation of new cardiomyocytes and by improving the survival of preexisting cardiomyocytes. This resulted in the decrease of left ventricle infarct size, improvement of left ventricle dilatation and wall stresses, and decrease of left ventricle hypertrophy.
However, obstacles to clinical translation remain. The study used open-heart intramyocardial injection of cardiomyocyte SMRTs immediately after an experimental heart attack. This method is not readily applicable in clinical practice, and other approaches also have limitations, say Zhang and Zangi.
“Currently, direct intravascular or intracoronary injection of the cardiomyocyte SMRTs is unlikely to be maximally effective, because mRNA is rapidly degraded by RNase in the circulation,” Zhang said. “Although lipid nanoparticle-encapsulated modified RNA is FDA-approved and sufficiently stable to ensure that the modified RNA is taken up by cells, most systemically injected lipid nanoparticles home to the liver. To realize the full potential of modified RNA-based gene therapy for patients, different delivery methods such as cardiac-targeted lipid nanoparticles and different time points — weeks or months after heart infarct induction — will need to be developed and tested.”
Co-first authors of the study, “CCND2 modified mRNA activates cell cycle of cardiomyocytes in hearts with myocardial infarction in mice and pigs,” are Jiacheng “Jason” Sun and Lu Wang.
Co-authors with Zhang, Zangi, Sun and Wang are Rachel C. Matthews, Gregory P. Walcott, Yu-An Lu, Yuhua Wei and Yang Zhou, UAB Department of Biomedical Engineering.
Support came from National Institutes of Health grants HL114120, HL131017, HL149137, HL134764, HL160476 and HL153220; American Heart Association Transformational Project Award 969529 and American Heart Association grants 20PRE35210006 and 23PRE1025367.
At UAB, Biomedical Engineering is a joint department of the Marnix E. Heersink School of Medicine and the School of Engineering, and Zhang holds the T. Michael and Gillian Goodrich Endowed Chair of Engineering Leadership.