 Vaccination of neonatal mice with group A Streptococcus promotes clonal expansion of B cells that produce antibody against GlcNAc. The association of reduced Type 1 diabetes risk after group A Streptococcus infection is dependent on these GlcNAc-specific B cells.Researchers have discovered the novel mechanism that underlies a previously reported observation that infection by group A Streptococcus bacteria reduces the risk of later developing Type 1 diabetes.
Vaccination of neonatal mice with group A Streptococcus promotes clonal expansion of B cells that produce antibody against GlcNAc. The association of reduced Type 1 diabetes risk after group A Streptococcus infection is dependent on these GlcNAc-specific B cells.Researchers have discovered the novel mechanism that underlies a previously reported observation that infection by group A Streptococcus bacteria reduces the risk of later developing Type 1 diabetes.
The Journal of Immunology reports that vaccination of neonatal mice with group A Streptococcus promoted a clonal expansion of innate-like B cells that produce antibody against N-acetyl-D-glucosamine, or GlcNAc. GlcNAc is a derivative of glucose sugar that is found as part of the cell wall of group A Streptococci and as part of antigens on the insulin-producing pancreatic beta cells that are formed by GlcNAc posttranslational modifications.
The University of Alabama at Birmingham researchers showed that the associations of reduced Type 1 diabetes risk after group A Streptococcus infection was dependent on these GlcNAc-specific B-1 B cells. B-1 cells in mice are a type of B cell that produces natural antibodies, which are antibodies produced without infection. Such natural antibodies can aid in producing tolerance, the process where the immune system learns to tolerate — not attack — its own tissues.
This finding of the role for B-1 B cells “demonstrates the potential for targeting the natural antibody repertoire in considering therapeutic strategies for Type 1 diabetes,” said John Kearney, Ph.D., a professor in the UAB Department of Microbiology, who led the study.
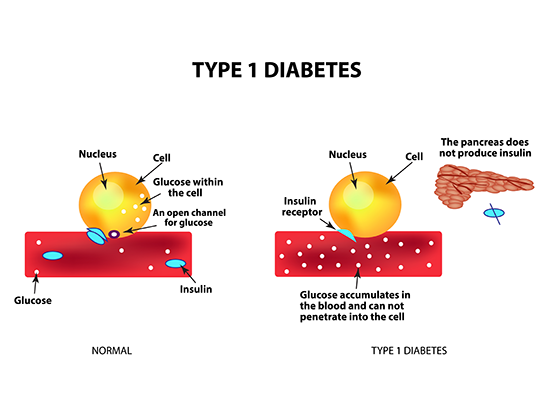
Autoimmune diseases like Type 1 diabetes are a failure to maintain tolerance. In Type 1 diabetes, the immune system attacks and specifically destroys the insulin-producing beta cells in the pancreas. Insulin is the hormone that helps cells use glucose for energy. The loss of insulin production after death of beta cells creates damaging high levels of glucose in the blood that can lead to disabilities, including blindness, heart disease and kidney failure.
Similar to the findings of others, the UAB researchers first showed immunization of neonatal mice at 14 days of age with dead or living group A Streptococcus protected them from Type 1 diabetes, as compared to controls. In contrast, adult immunization of this mouse strain, which is prone to develop diabetes, failed to protect, so timing was central to protection.
At 10 to 12 weeks of age, the naïve mice with diabetes had significant B and T cell infiltration into the pancreas and a breakdown of the membrane around the pancreatic islets that contain beta cells. The mice that were neonatally immunized did not show those pathological changes.
The neonatally immunized mice produced immunoglobulin M, or IgM, that bound to both group A carbohydrate and GlcNAc, and the mice also showed a clonal expansion of otherwise low frequency group A carbohydrate-reactive B-1b B cell clonotypes.
The UAB researchers created group A carbohydrate-reactive monoclonal antibodies to probe possible targets of the IgM antibodies, and they found that the monoclonal antibodies recognized insulin secretory granule-associated GlcNAc antigen portions, known as epitopes, on pancreatic beta cells. These group A carbohydrate-reactive monoclonal antibodies had robust reactivity for both human and mouse pancreatic islets.
These epitopes appeared to be generated during autophagosomal degradation of mature carbohydrates, one of the steps of apoptosis, or the programmed cell death, of beta cells. Experiments showed that the GlcNAc-reactive B cell response to group A streptococci appeared to delay Type 1 diabetes, potentially by facilitating efficient clearance of apoptotic beta cells, thereby limiting activation of killer and helper T cells that ultimately would destroy healthy beta cells. Indeed, ex vivo experiments showed that binding of group A carbohydrate-reactive monoclonal antibodies to pancreatic islet cells inhibited T cell activation.
 John Kearney, Ph.D.However, there was a mystery.
John Kearney, Ph.D.However, there was a mystery.
Administration of antibody alone, either a monoclonal antibody or pooled IgM from immunized mice, failed to protect naïve mice from developing Type 1 diabetes. Thus, while the IgM producing B cells are central to inhibiting Type 1 diabetes, and while the IgM antibody protects against T cell activation in test tube experiments with isolated cells, the IgM by itself was not able to protect naïve mice from developing Type 1 diabetes.
The answer to this mystery is that the group A carbohydrate-reactive B-1 B cells show a striking propensity to infiltrate the pancreas as Type 1 diabetes begins to develop in the mice. At 10 to 12 weeks of age, neonatal immunization had increased the numbers of activated group A carbohydrate-positive B cells uniquely localized in the pancreas by 20-fold. There, the researchers suggest, the B cells can produce IgM or other possible soluble mediators that protect the beta cells.
While IgM alone was not protective, the researchers further found that adoptive transfer of B cells from mice that were neonatally immunized with group A carbohydrate has the ability to significantly reduce the incidence of Type 1 diabetes in recipient mice at 30 weeks of age.
“Collectively, our observations indicate a significant involvement of cryptic glycan epitopes in immunological recognition of senescent beta cells, and that clonal composition of the GlcNAc-specific B cell repertoire during early life can significantly influence immune responsiveness to Type 1 diabetes autoantigens,” Kearney said. “We postulate that natural antibody repertoire defects precede emergence of beta cell-specific autoantibodies associated with and currently used to determine the risk of Type 1 diabetes progression.”
J. Stewart New is lead author of the study, “B-1 B cell–derived natural antibodies against N-Acetyl-D-Glucosamine suppress autoimmune diabetes pathogenesis,” which editors of The Journal of Immunology selected as a Top Read in the Nov. 1 issue.
Co-authors with New and Kearney are Brian L.P. Dizon and R. Glenn King, UAB Department of Microbiology; and Neil S. Greenspan, Case Western Reserve University, Cleveland, Ohio.
Support came from National Institutes of Health grants AI4782, AI120500, AI007051, DK082227 and GM008861; and Juvenile Diabetes Research Foundation grants 2-SRA-2014-300-Q-R and 17-2012-123.
At UAB, Microbiology is a department in the Marnix E. Heersink School of Medicine, and Kearney is a Distinguished Professor of Microbiology.