 The 3rd Annual CCTS Bioethics Forum speakers: (l to r) AGHI PI and CCTS Director of Genomic Medicine Dr. Bruce Korf, AGHI Recruitment Manager Julie Schach, AGHI Study Navigator Angela Williams, CCTS Bioethics Expert Dr. Stephen Sodeke, Bioethics Professor Dr. Mariko Nakano, AGHI Program Director Renie Moss, and CCTS Training Academy Co-Director Dr. David Chaplin.
The 3rd Annual CCTS Bioethics Forum speakers: (l to r) AGHI PI and CCTS Director of Genomic Medicine Dr. Bruce Korf, AGHI Recruitment Manager Julie Schach, AGHI Study Navigator Angela Williams, CCTS Bioethics Expert Dr. Stephen Sodeke, Bioethics Professor Dr. Mariko Nakano, AGHI Program Director Renie Moss, and CCTS Training Academy Co-Director Dr. David Chaplin.
What is trust? What helps build or derail it? Why does it matter to research participants, to investigators? How can a research institution demonstrate trustworthiness to potential participants? What does equitable, ethical participation in research by underrepresented populations look like? And what methods can be used to measure the effectiveness of efforts to develop trust and trustworthiness in research?
These thought-provoking questions formed the basis of the 3rd Annual CCTS Bioethics Forum, which took place on Friday, March 16, 2018. The speakers, including CCTS Bioethics Expert and Tuskegee Bioethicist and Professor of Allied Health Dr. Stephen Olufemi Sodeke, UAB Assistant Professor of Bioethics Dr. Mariko Nakano, and Co-Manager of Recruitment and Retention Shared Facility Julie Schach, set an ambitious agenda: to explore the role of trust and trustworthiness in eradicating barriers to participation in genetic and genomic research.
 A word cloud created in real time via text answers to “what words come to mind when you think of trust and trustworthiness?” Honesty, transparency, and respect topped the list.
A word cloud created in real time via text answers to “what words come to mind when you think of trust and trustworthiness?” Honesty, transparency, and respect topped the list.
A History of Betrayal
Using an array of interactive exercises, videos, and other dialog prompts, the speakers guided attendees through two key historically relevant research projects that betrayed the trust of their participants: the Tuskegee Syphilis Study (TSS) and the Diabetes Project with the Havasupai Tribe. Both resulted in major changes in how research is currently conducted using established Institutional Review Boards (IRB) and informed consent procedures. A migration study based on unauthorized use of the Havasupai blood samples also raised the issue of the need for protection of genetic information for groups as well as individuals.
 The AGHI presentation underscored the value of incorporating bioethics in the earliest planning stages of a genomics study.
The AGHI presentation underscored the value of incorporating bioethics in the earliest planning stages of a genomics study.
Sodeke shared an excerpt from a speech by Mr. Herman Shaw, spokesperson for TSS survivors, given at the Apology Ceremony held by the Clinton Administration in 1997. Shaw stated that the damage inflicted by the unethical treatment of the African American airmen and their families was far deeper than any physical wounds suffered, indicating that the legacy of distrust in medical research was still vivid decades later. “Investigators must realize they are starting from a ‘Give me a compelling reason why I should trust you?’ basis,” Sodeke said.
Despite the historical distance, both cases underscore the moral tension that exists between researchers and participants. Even if research is conducted ethically by today’s IRB standards, Sodeke noted, trust can be difficult to establish and is easily lost, to the detriment of improved health outcomes for all concerned. “We need a glimpse of imagination to go beyond regulation, beyond merely doing what the IRB tells us we must do. Regulations are the floor, not the ceiling.”
A Bioethics Paradigm Shift: The Alabama Genomic Health Initiative (AGHI)
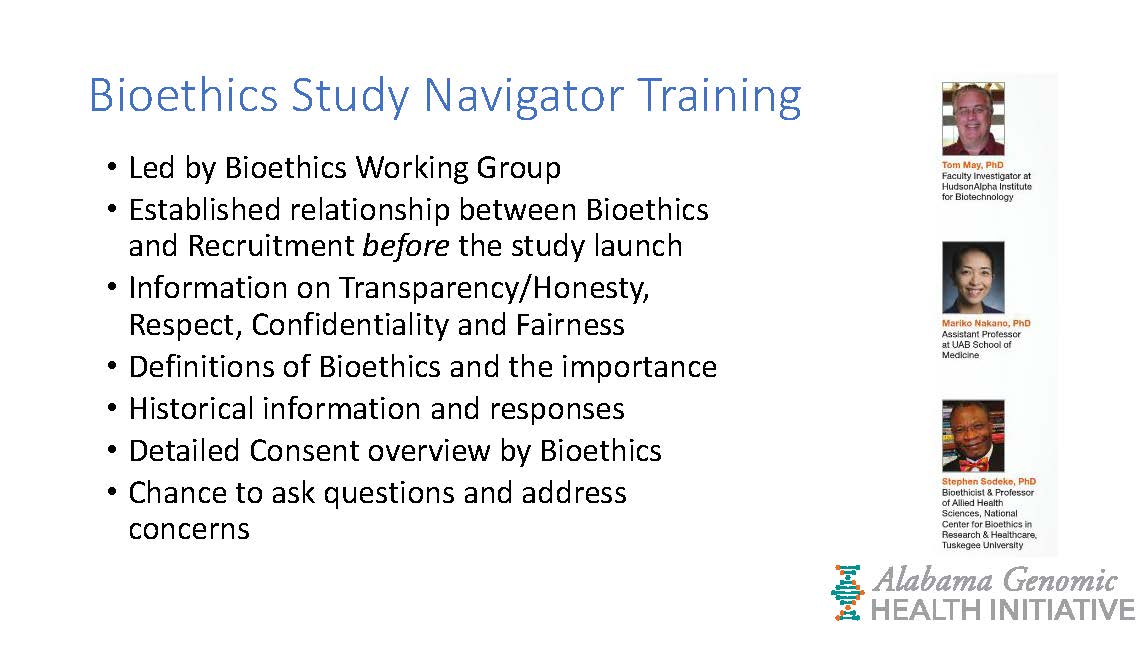 A list of the many ways bioethics experts contributed to training patient navigators and ensuring the AGHI recruitment process was transparent, ethical, and trustworthy.
A list of the many ways bioethics experts contributed to training patient navigators and ensuring the AGHI recruitment process was transparent, ethical, and trustworthy.
The AGHI, led by CCTS Director of Genomic Medicine and UAB Chief Genomic Officer Dr. Bruce Korf, was explored next as an example of a study that is going the extra mile to build and maintain trust. The project, which involves CCTS Partners UA, USA, HudsonAlpha and the Hub in collaboration with UAB branch programs in Montgomery, Selma, Huntsville, and Cooper Green, aims to test the blood samples of 10,000 Alabamians for 59 genes associated with treatable medical conditions. To ensure the state's diverse population is accurately represented, regaining trust was the foremost concern, according to ethicist and UAB School of Medicine Assistant Professor Dr. Mariko Nakano.
AGHI Recruitment Manager Julie Schach described the many steps taken to inspire and maintain trust, including involving bioethics experts in the protocol and recruitment design process; ensuring the informed consent process was “plain language” and clear to all participants regardless of education level; and including the use of community health advocates as study navigators to ensure participants understand the purpose of the study and the choices they have concerning results and how their data will be used in the future. Angela Williams, one of AGHI’s study navigators, further discussed the process for guiding potential participants through the 13-page informed consent document.
 Participants in AGHI have the power of choice over their data, including who sees their results and if they may be used in a future study.
Participants in AGHI have the power of choice over their data, including who sees their results and if they may be used in a future study.
Next Steps: A Dialogue
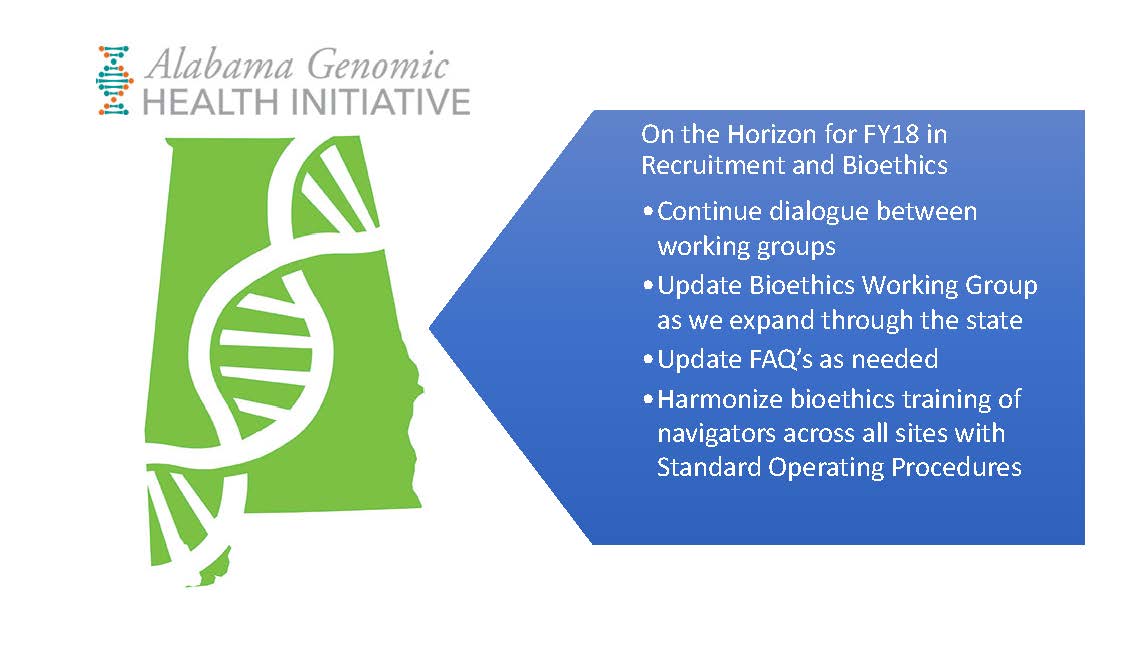 The Bioethics Working Group continues to work with the AGHI principal investigators to ensure the same ethical standards apply to recruitment in all Alabama sites.
The Bioethics Working Group continues to work with the AGHI principal investigators to ensure the same ethical standards apply to recruitment in all Alabama sites.
Although AGHI’s approach represents a far more rigorous level of ethics in population-based genomics research, the audience raised many questions that highlighted remaining trust challenges: Who selected the 59 actionable diseases targeted by AGHI and by what criteria? Why use a broad consent for future use of data instead of contacting subjects each time their data will be reused? Is a 7th grade language level for the informed consent process sufficient to ensure low literacy participants truly understand their risks and rights?
Korf fielded these and other questions, briefly describing the logistical, budgetary, and regulatory realities involved in running a state-wide research project. He emphasized four principles guide all AGHI decisions: transparency, respect, confidentiality, and fairness.
Sodeke reminded the group that “even when warranted, trust is risky and dangerous.” CCTS Training Academy Co-Director Dr. David Chaplin, who facilitated the workshop, agreed challenges remain, noting current events reflect a general sense of distrust in institutions. A participant agreed, suggesting “perhaps we should focus on how to make research institutions more trustworthy instead of expecting potential subjects to trust individual researchers.”
“We must be co-creators of where we go from here,” Sodeke concluded, promising “this dialogue will continue.”
In case you missed it: a video of our 3rd Annual Bioethics Forum will soon be available on the CCTS YouTube channel. The speakers’ slide decks are available below. Subscribe to CCTS Digest to find out about our upcoming events and learning opportunities.
For a deeper look at AGHI’s approach to bioethical issues and why it matters, see UAB Magazine’s “The Ethics of Genetics,” by Matt Windsor.
3rd Annual CCTS Bioethics Forum Slide Decks:
3rd Annual CCTS Partnership Bioethics Forum: Trust and Trustworthiness Series
Alabama Genomic Health Initiative: Current Experiences with Barriers to Participation: The AGHI Example