Leading PIs from the Alabama Genomic Health Initiative (AGHI) and the Jackson Heart Study shared lessons learned concerning RoR. Many revolved around unanticipated reactions to the process for returning results. Participants sometimes requested more information, such as the entire raw data set of their genetic results, than researchers were prepared to provide. Others balked at sharing even actionable results with their primary care physicians.
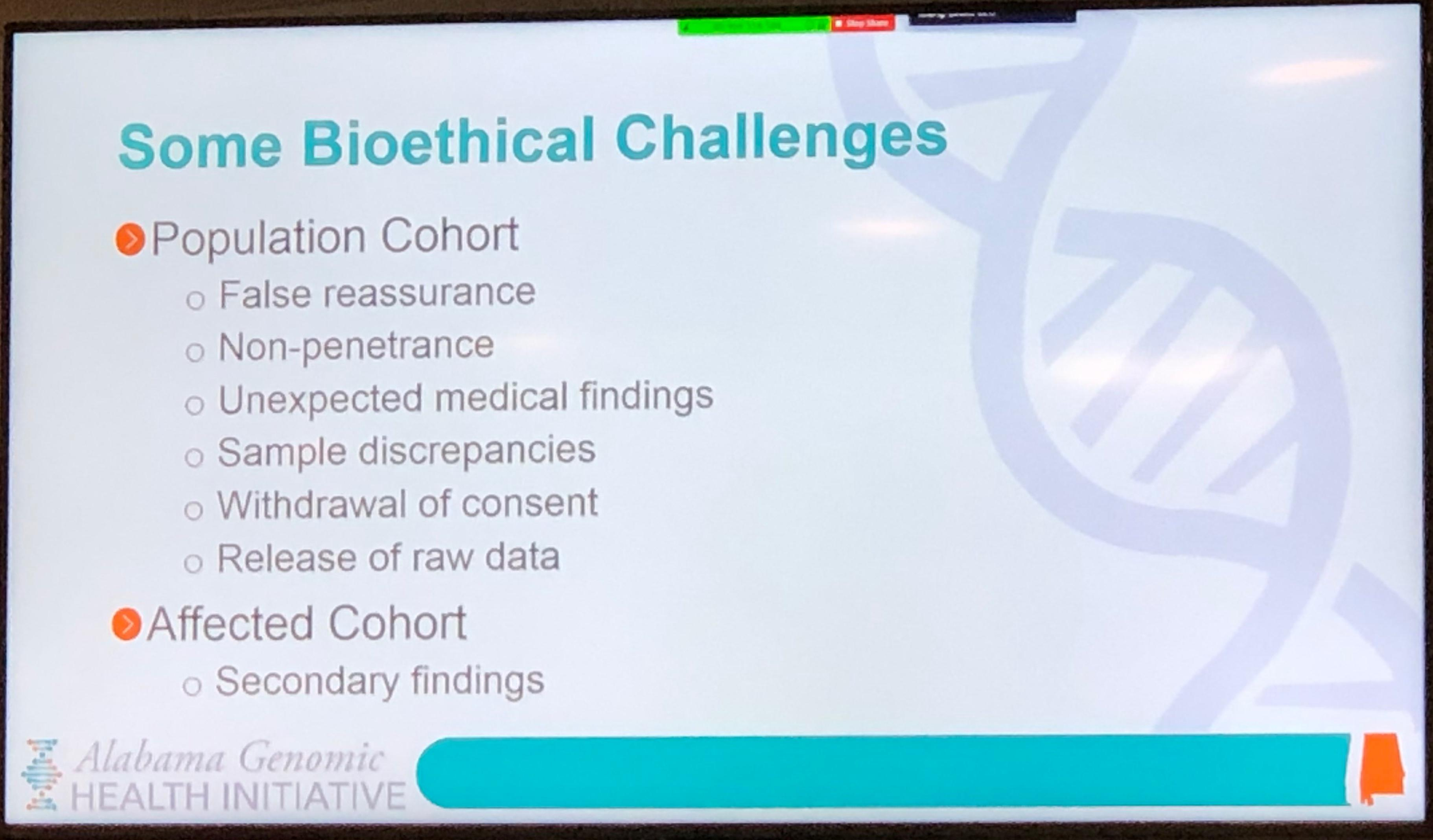
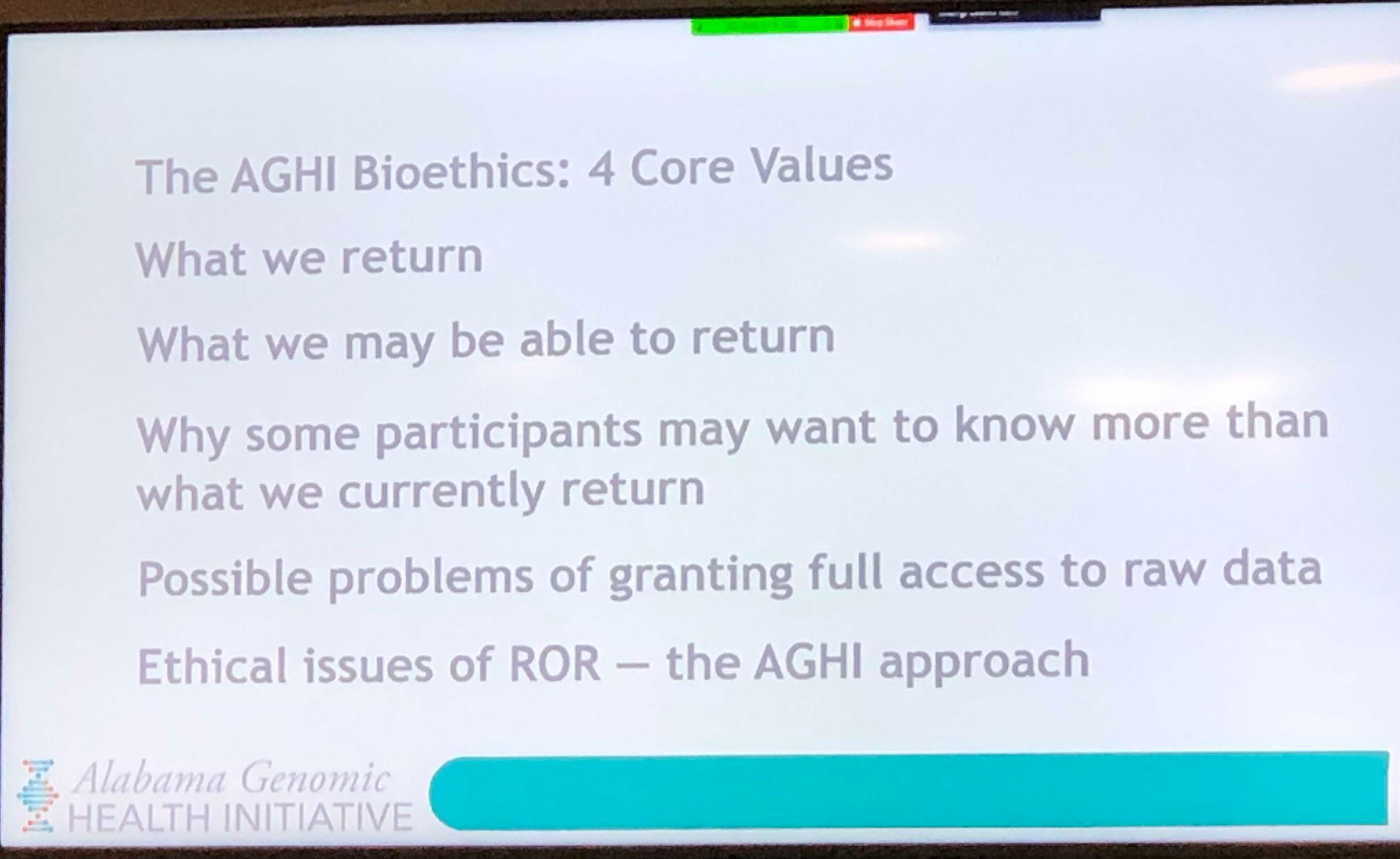
Dr. Mariko Nakano, Assistant Professor of Bioethics at UAB’s School of Medicine, led a session on other bioethical challenges in RoR, including expectations fueled by commercial products such as 23andMe. Participants sometimes expect clinical and genetic studies to return medically non-actionable results, carrier status, non-medical biological traits, and ancestry-related information.
Unlike commercial products, academic research studies have more constrained budgets and Hippocratic concerns about doing harm by confusing patients with results that may lack 100% scientific accuracy and clinical certainty. “Many genetic variants show incomplete penetrance, for instance, but this is a difficult genetic concept for the general public to understand,” said Nakano. [Editor’s note: Penetrance is the extent to which a particular gene or set of genes is expressed in the phenotype of individuals carrying it, as measured by the proportion of carriers showing the characteristic phenotype.] Genetic counselors are a critical part of the RoR process for those with actionable results, as they are trained in explaining such concepts.
A special panel discussion featuring several AGHI participants underscored the complexity of bioethical challenges in RoR with the variability of their experiences and perspectives. Although all four participants consented to sharing their results with their primary care physicians and with the biobank for future research, they differed on sharing results with family members, their preference for knowing when to expect results, how well they understood the informed consent process, and how anxious they felt after talking to a genetic counselor about a positive result.
Dr. Adolfo Correa, PI of the Jackson Heart Study, the largest single site, community-based study of cardiovascular disease among African Americans, agreed that one of the biggest challenges in RoR was how little is known about the impact on participants. “What are the health benefits? What are the risks, including psychosocial, financial, and familial? We need to do a better job of preparing participants for the return of their genetic information,” he said.
Tuskegee University Resident Bioethicist and Professor of Bioethics Dr. Stephen Olufemi Sodeke led the Forum’s final session, reminding the audience of the many historic reasons communities of color have for distrusting research and how fraught the RoR process is for eroding progress in trust. He conducted an exercise to brainstorm practical steps for promoting trust and trustworthiness among collaborating institutions and those volunteering for research. The top seemingly simple recommendation? Communication.
CCTS thanks our bioethical experts for their highly informative and thought-provoking Forum presentations and our Bioethics Forum planning committee (listed below) for developing an outstanding event. A special thank you goes out to our Training Academy Program Director Dr. Becky Reamey and Co-Director Dr. David Chaplin for their programmatic, logistical, and promotional support and to our AGHI participants for sharing their RoR experiences with our live audience.
Several sessions of our 4th Bioethics Forum are available for viewing on the CCTS YouTube channel. To maintain the privacy of their health information, the panel discussion featuring AGHI participants was not recorded.
4th Bioethics Forum Planning Committee
David Chaplin, MD, PhD
Bruce R. Korf, MD, PhD
Chiquita Lee, BS, MBA
Mariko Nakano, PhD
Becky Reamey, PhD
Stephen Olufemi Sodeke, PhD, MA
Clayton Yates, PhD
Slide Decks: Dr. Korf, Dr. Nakano