 |
Gorgas Case 2016-02 |
 |
|
The following patient was seen in the inpatient department of the 36-bed Tropical Disease Unit at Cayetano Heredia National Hospital in Lima, Perú.
 History: 21-year-old previously healthy male presents to the ER with a 6-day history of illness. Symptoms included: fever of unknown intensity for the first two days; headache (8/10 intensity); left flank pain radiating to his back; and shortness of breath beginning on the second day of illness. Fatigue, somnolence, anorexia, nausea and repeated vomiting ensued, leading to oral intolerance over the next 3-days. The family reported that he complained of a 3-kg weight loss, absence of bowel movements, dark urine and they noted jaundice the day of his admission. No history of skin rash, joint pain, genitourinary symptoms or bleeding. Received unknown over the counter analgesics and antipyretics during the illness.
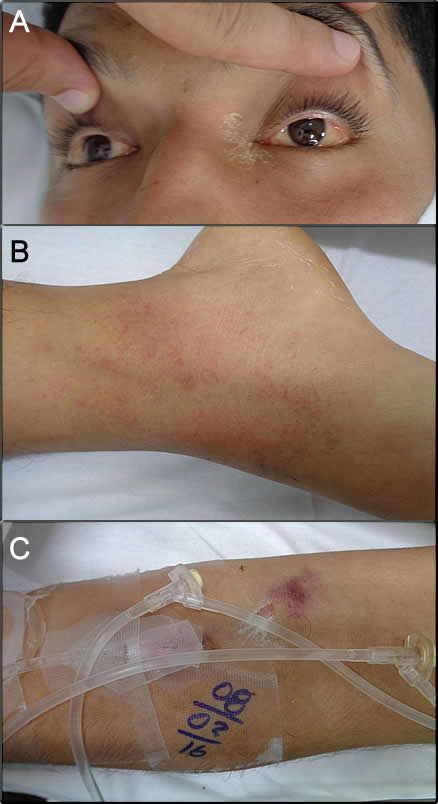
Epidemiology: Born and lives in Lima with his family, works at a printing house. No smoking, alcohol or illicit drug use. No known TB exposure. All routine vaccines including Hepatitis B up to date. Returned to Lima with his girlfriend 2 days prior to illness onset after a 2-day trip to Chanchamayo, a high jungle area of Peru. Stayed in city, used repellent but no use of mosquito nets at night, went on a full-day hike in the jungle with exposure to fresh water, he walked barefoot in the mud, noticed no rodents. Had no pre-travel advice, vaccines or malaria prophylaxis. Physical Examination: HR 102; RR 29; BP 120/63; T 37.2°C; SO2 100% (FiO2 21%) Patient in acute distress. Skin pallor and scleral icterus (Image A), petechial rash on ankles and dorsum of both feet (Image B), ecchymosis at venipuncture sites (Image C), capillary refill <2 sec. No edema, no lymphadenopathy. Normal heart and lung exam. Abdomen: distended, normal bowel sounds, tenderness to palpation of the right upper quadrant, liver felt 3cm below right costal border. Unremarkable neurologic exam. Laboratory Examination (on admission): Hb 17.8 g/dL, WBC 5.5 (0 bands, 4.11 neutrophils, 0.03 eosinophils, 0.02 basophils, 0.39 monocytes, 0.95 lymphocytes), platelets 180 000. PT 45.1” (INR 5.22), fibrinogen 126 mg/dL (N: 200-400), β2-microglobulin 8.98 ug/ml (N<2.7). Glucose 68 mg/dL, urea 139.3 mg/dL, creatinine 9.0 mg/dL. Na+ 132 mEq/L, K+ 5.8 mEq/L, Cl- 99 mEq/L. Total bilirubin 7.2 mg/dL (conjugated 6.2 mg/dL). AST 14 954 U/L, ALT 8 889 U/L, AP 241 U/L, GGT 174 U/L, CPK 891 U/L (N<170), CPK-MB 20 U/L (N: 0 -16) Urinalysis: protein 100mg, glucose 50mg, RBC 29/hpf, WBC 6/hpf. 12-hour urine output: 50 cc. Other tests: Thick smear for malaria negative x2.
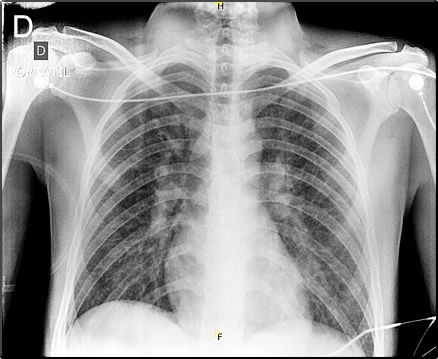
|
|
Diagnosis: Viral hemorrhagic fever due to Yellow Fever.
 Discussion: ELISA IgM for Yellow fever on day 6 of illness was positive at NIH-Peru. PCR and culture were not performed. HBsAg and Anti HBc negative, HBsAg-Ab positive (vaccinated), Anti HCV negative, IgM for hepatitis A negative, ELISA IgM and IgG for Dengue negative. IFI IgG Ab and total Ab for Rickettsia negative. IgM leptospira negative, at the NIH-Peru. IgM for yellow fever typically is positive by day 7 of illness compared to day 5 for a dengue IgM. Fulminant yellow fever is the true prototypical viral hemorrhagic fever (unlike Ebola Virus Disease in the recent African outbreak) where patients bleed out and the liver dissolves [see recent review of yellow fever in J Clin Virol. 2014 Oct 24. pii:S1386-6532(14)00369-2]. Pathophysiological features are shared with several unrelated diseases except that the severity and extent of the hepatonecrosis is greatest in yellow fever patients. The hallmarks of the full yellow fever syndrome include the pathognomonic triad of hemorrhagic fever with jaundice and renal disease. Other viral hemorrhagic fevers may present with either jaundice or with renal disease, but the combination should always suggest yellow fever if there has been appropriate exposure according to the epidemiologic history. • Dengue hemorrhagic fever is co-endemic in many areas but the pathophysiology is related to increased capillary leakage and illness is usually accompanied by a history of rash at some point in the illness. Hepatitis occurs only occasionally and is mild. Renal involvement does not occur with dengue and the finding of significant proteinuria (such as in this case) on a urine dipstick should always suggest yellow fever over dengue even early in the course of the clinical evolution. Mild cases of yellow fever cannot be distinguished clinically from falciparum malaria, leptospirosis, viral hepatitis, typhoid, rickettsial disease, hepatotoxin ingestion, or relapsing fever. More than 80% of yellow fever infections are symptomatic and the incubation period is usually very short, 3 to 6 days. After an acute febrile illness with headache and myalgia without rash, which likely represents the peak viremia, there may be a period of remission. Severe cases most often do not follow that course and progress quickly to multi-organ failure with liver failure as the main determinant of mortality. Severe oliguric renal failure very early in the course as in this case is unusual. With biphasic illness, fever may then resume with back pain, nausea, vomiting, and mental status changes. Black vomitus (hematemesis) is commonly described. In fatal cases death usually occurs 6 to 10 days into the illness. Pathologically, yellow fever causes hepatocellular and Kupffer cell infection. There is mid-zonal hepatocellular necrosis with a minimal inflammatory response. So-called Councilman bodies and microvesicular fatty change is seen. A marked decrease of hepatic transaminases and bilirubin just before death likely represents near total destruction of functioning hepatocytes. In our patient, transaminases decreased from a peak of 300 times normal to 10 times normal (see below). In 2014, 17 yellow fever cases were confirmed in Perú, with 7 in San Martin and 2 in Junin (Chanchamayo). In 2013 there were 21 cases with a case-fatality rate of 64%. The total number of reported cases in Chanchamayo is decreasing in recent years. In many recent years Perú has reported more cases of yellow fever than other countries in South America combined; this may reflect the excellent surveillance system. As with other flaviviruses there is no specific treatment for yellow fever, making prevention by use of 17D yellow fever vaccine (essentially 100% effective) imperative. Most individuals in endemic areas (Amazon basin and sub-Saharan Africa) have variable access to vaccines but the much higher general vaccine coverage in endemic areas of Latin America account for the relatively few annual cases compared to 50,000/yr in Africa. Nonetheless, there is dramatic under-use of vaccine by travelers and expatriates. At least 10 unvaccinated short-term travelers to endemic areas have died of yellow fever since 1995. Data indicates that the number of unvaccinated travelers visiting risk areas is substantial. In Perú specifically, government vaccination programs cover the endemic areas, but residents of non-endemic areas who travel to the jungle are often poorly informed of the risk. Soon after presentation, the patient developed respiratory distress with the following lab parameters: Arterial blood gases: pH 7.30, pCO2 18.4, pO2 49.2, SO2 77.9 (FiO2 of 21%, PO2/FiO2: 234), HCO3 9.0, serum lactate 5.0. Pulmonary involvement early on the course of illness is also seen, the majority of patients then develop ARDS. Chest X-ray from the ER is shown (Image D). After intubation and mechanical ventilation, interventions included acetylcysteine, fresh frozen plasma, dialysis, RBC and cryoprecipitate transfusions were instituted for the typical coagulopathy in this disease. Bleeding through the dialysis catheter insertion site (up to 800cc) and coffee grounds through the orogastric tube (up to 200cc) ensued. Nosocomial pneumonia with Acinetobacter ensued despite empiric antibiotic therapy from the outset and he remains stable but intubated and remains on dialysis. Liver function has stabilized but may reflect massive hepatic destruction. Total bilirrubin 6.2 mg/dL (conjugated 3.4 mg/dL, unconjugated 2.8 mg/dL). AST 189 U/L, ALT 361 U/L, AP 119 U/L, GGT 265 U/L, LDH 1177. Both other yellow fever cases seen during earlier Gorgas Courses (2015-2; 2002-10) have been fatal. Of note, his girlfriend was admitted one day later with a milder febrile illness, serology for yellow fever was also positive. She is recovering uneventfully. Sexual transmission has not been reported in yellow fever. By report the 2 patients did not have sexual relations during or after the trip. |