 |
Gorgas Case 2016-06 |
 |
|
The following patient was seen in the inpatient department of the 36-bed Tropical Disease Unit at Cayetano Heredia National Hospital in Lima, Perú.
 History: 39-year-old MSM presented to the outpatient clinic to re-start anti-retrovirals. He was diagnosed with HIV infection 14 months previously when he presented with P. jirovecii pneumonia and was treated succesfully with 21 days of trimethoprim/sulfa (CMX) and prednisone. CD4 cell count at that time was 125 cells/mm3 and a viral load was not obtained. CMX prophylaxis was continued for a few months, but ART and medical contact was discontinued after 1 month. For the previous 4 months he had noticed several painless violaceous skin lesions on the trunk and extremities and also dry cough without constitutonal symptoms. History of an anorectal fistula at the same time as the initial presentation.
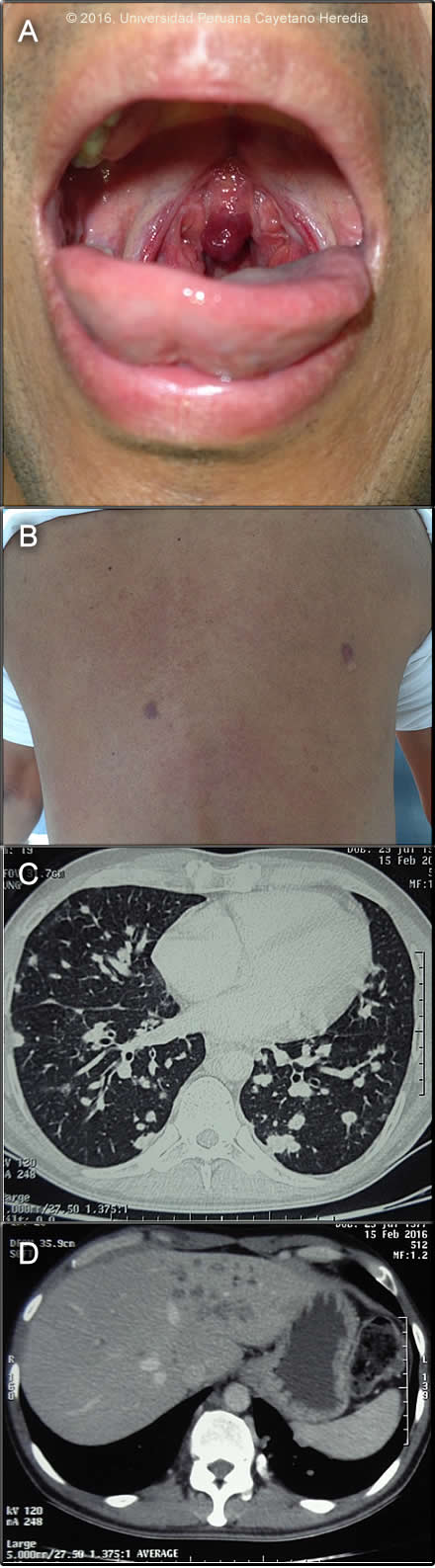
Epidemiology: Born and lives in Lima and is an accountant. No known TB contact history. Travel to Cuzco 3 months before re-presentation. Physical Examination: T 36.5. RR 14; pulse 76; BP 100/64; BMI 23.17. HEENT: violaceous infiltrative lesion of the uvula (Image A), 11 papular, violaceous lesions located on the trunk and extremities (Image B). No lymphadenopathy. Chest: few rales in both lungs. Abdomen: no hepatosplenomegaly. Laboratory Examination (on admission) and Imaging:CD4 cell count: 34 cells/mm3 ; viral load is pending. Hemoglobin: 10.7, Hematocrit: 32%, WBC: 4.78K, Neutrophils:59%, Lymphocytes: 32, Platelets: 282K. Glucose: 97, Creatinine: 0.9; AST: 31, ALT: 37. Total Protein: 6.9. Albumin: 4, Total Bilirrubin: 0.4, Alkaline Phosphatase: 331 (elevated). Sputum AFB: negative x 3. AFB culture (MGIT): negative. HTLV1: not reactive; RPR not reactive. CT scan of the chest and abdomen are shown (Images C & D). CEA 1.79 (normal)
|
|
Diagnosis:Kaposi`s sarcoma (KS due to HHV8); HIV associated.
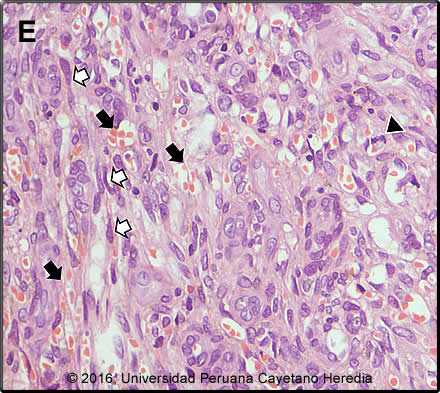
 Discussion: Biopsy of a skin lesion showed (Image E): microvascular proliferation (varying vessel shape and size with vascular congestion and RBC extravasation (black arrows); spindle cells (sarcomatoid cells) with pale eosinophilic cytoplasm and oval elongated nuclei (white arrows); occasional mitotic figures (arrow head). These 3 findings together are diagnostic of KS. CT scan of the chest (Image C) was read as showing multiple nodular lesions of different sizes located in both lungs and the CT scan of the abdomen (Image D) as showing hypondense lesions of the liver. GI endoscopy and colonscopy showed multiple violaceous lesions in the small and large intestine (images not available). Bronchoscpy did not show any endobronchial lesions and KOH, Grocott and ZN of the BAL were negative as were MGIT cultures for MTB and cultures for other mycobacteria. Latex agglutination test Cryptococcus was negative and histoplasma and paracoccidiodomycis immunodiffusion were negative. Culture for nocardia was negative. The differential diagnosis of the skin lesions in this patient includes mainly bacillary angiomatosis due to Bartonella; the biopsy helps in distnguishing these conditions, and a Waathin-Starry stain would indentify clumps of bacteria in bacillary angiomatosis. The differential diagnosis of pulmonary nodules in patients with HIV is broad and includes TBC, nocardia which is usually associated with skin lesions that look like nodules and abscesses, and fungal pathogens including histoplasma, paracoccidiodomycosis and cryptococcus Pneumocystosis rarely presents with nodules. Cancer including KS (the most likely), lymphoma, and metastatic cancer should also be considered. Kaposi’s sarcoma is caused by HHV-8 (human herpes virus 8) and was first described in Africa in the pre-HIV era. It is the most common HIV associated malignancy including in Latin America (J Acquir Immune Defic Syndr. 2011 April 15; 56(5): 467–473. doi:10.1097/QAI.0b013e31820bb1c3) and in some African countries with high HIV rates it is the most common malignancy in men. For unclear reasons though, it is uncommon in Asia. HHV-8 transmission routes are not totally clear and both sexual and horizontal nonsexual (mother to child; between siblings) HHV-8 transmission routes have been reported. Due to low general seroprevalence of HHV-8 in the population in developed countries and early initiation of anti-retroviral therapy, HIV-related KS is an infrequent condition in developed countries. Currently, KS is more commonly reported from developing countries than developed countries. HIV-infection is an important risk factor for developing KS in developing countries. HIV-infection is associated with an increased HHV-8 sero-prevalence in all population groups examined. Overall, HIV-positive persons are more likely to be HHV-8 seropositive than HIV-negative persons and the association is strongest in MSM, patients with hemophilia, and children (Int. J. Cancer: 138, 45–54, 2016). Co-infection with HIV and HHV8 is more frequent in males (reasons unclear), and is usually seen in severely immunosupressed patients, the lower the CD4 the higher the risk. Patients typically have a CD4< 200 cells/mm3 and history of an opportunistic infection such as pneumocystis. In patients who present with limited disease there is no indication to start chemotherapy; these patients will benefit from HAART (any regimen) alone (AIDS Reviews 7: 13-21, 2005). Clinically, this is a case of advanced poor-risk KS based on three criteria: 1) Tumor, T1 stage; 2) extensive disease that involves not only the skin but also mucosal membranes; 3) involvement of other non-lymph node viscera involved (lungs, GI tract and liver). Treatment of KS in HIV-infected patients depends on the stage of the tumor and number of skin lesions (this patient had less than 50) and presence of symptomatic disease. Considering the extensive involvement in this case and despite of the scarcity of symptoms chemotherapy was offered. 5-year survival in T1 disease has been approximated as 80% with HAART and chemotherapy but the extensive pulmonary disease in our patient speaks to a poorer prognosis in our experience. The standard of care in the developed world is liposomal anthracyclines (doxorubicin or daunorubicin), but these drugs are not available in most of the developing world (Cochrane Database of Systematic Reviews 2014, Issue 9. Art. No.: CD003256. DOI: 10.1002/14651858.CD003256.pub2). Alternatives are IV combination of vincristine + vimblastine, IV paclitazel or oral etoposide. The patient was started on paclitazel, as per local protocol, and ART (Atripla). |