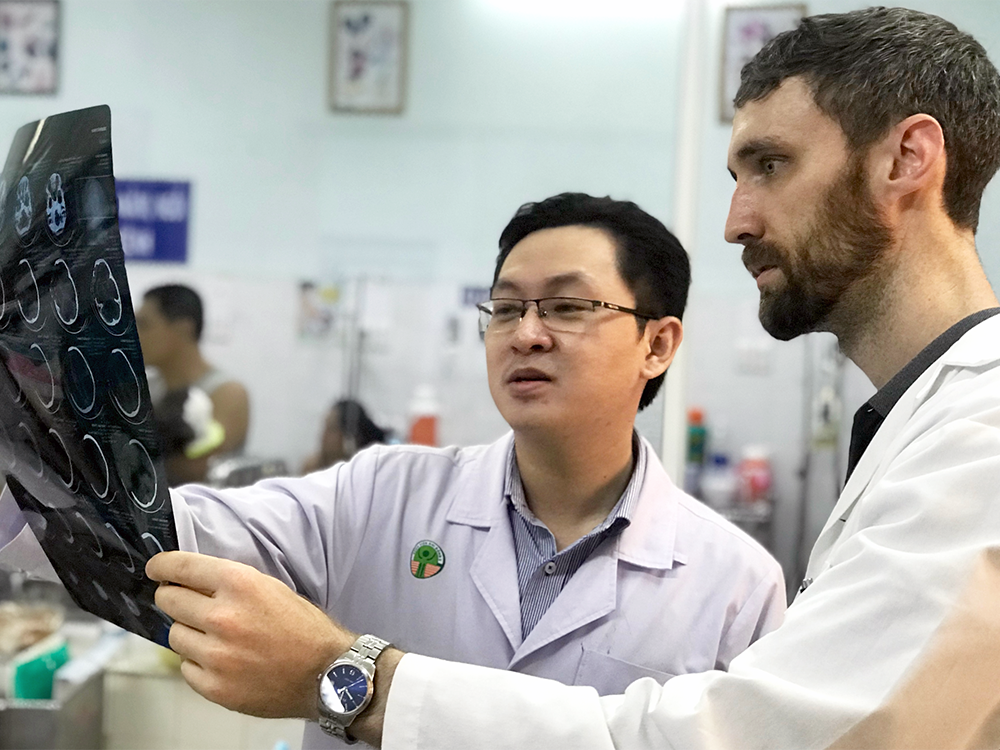
After spending nearly six months training in Ho Chi Minh City in Vietnam, UAB Department of Neurosurgery resident Jacob Lepard, M.D., returned to UAB this summer with a renewed sense of purpose and reverence for global neurosurgery.
 Dr. Jacob Lepard
Dr. Jacob Lepard
In May, Lepard completed the Paul Farmer Global Surgery Fellowship. The program, sponsored by Harvard Medical School and its Program for Global Surgery and Social Change, allowed Lepard to practice and conduct clinical research in both Uganda and Vietnam, where many still lack access to safe surgery.
Over the past year, Lepard’s fellowship has provided him with opportunities to learn from a number of Ugandan and Vietnamese surgeons and to continue his international training in the endoscopic management of hydrocephalus, a neurological disorder caused by fluid building within the brain. Through the fellowship’s two-part program, Lepard also spent two months treating and studying hydrocephalus at the Cure Children’s Hospital of Uganda last year.
“There’s really no amount of U.S. residency training that’s going to fully prepare you for what you see in Africa and Vietnam and other places because they just see things that we don’t see here,” Lepard said.
Lepard explained that the prevalence of hydrocephalus and other similar conditions within low- or lower-middle-income countries, such as Uganda and Vietnam, and the lack of available medical care for patients living with those conditions necessitate global health initiatives such as the Program for Global Surgery and Social Change.
“I think the fact that the vast majority of our population on earth, 5 billion people, don’t have access to safe surgery really makes it a moral imperative to solve this problem,” Lepard said.
Research published in the Lancet in 2015 reported that 143 million additional surgical procedures are still needed each year in low-income and lower-middle-income countries in order to meet the medical needs of the patients who live there.
“That number is kind of unfathomable to think of,” Lepard said. “In the U.S., if you have appendicitis, you go to the hospital, and you get your appendix taken out. If you get in a car wreck and you have an epidural hemorrhage, you go to UAB or somewhere else, and a neurosurgeon takes care of you. In other places, you simply don’t have access to that, so the alternative is that you don’t survive.”
Due in part to travel support provided by the UAB Neurosurgery Women's Leadership Council, Lepard most recently traveled to Vietnam, primarily working at Children’s Hospital Number 2 in Ho Chi Minh City.
Children’s Hospital Number 2 is one of three pediatric hospitals located in Ho Chi Minh City under the leadership of pediatric surgeon, Dang Do Thanh Can, M.D., who is no stranger to the challenges associated with limited access to surgical care.
“Dr. Can is the only pediatric surgeon in southern Vietnam, so he serves a population of about 13 million children,” Lepard said. “That kind of volume is just unheard of in high-income settings.”
Because Vietnam and other low-income or lower-middle-income countries continue to face a lack of access to safe surgery, many surgeons and neurosurgeons throughout the world have developed a global response to this crisis.
The Bogotá Declaration on Global Neurosurgery is one of the first calls to improve the availability of safe neurosurgery on a major scale. This declaration asks neurosurgeons to work toward improving neurosurgical conditions worldwide, and support for this initiative continues to increase as neurosurgeons organize to tackle this deficit in the accessibility of surgical care.
“The push for global neurosurgery initiatives like this is definitely a step in the right direction,” Lepard said. “You can’t just choose one disease in one area to focus on if you want to improve access to medical care for everyone. You have to build real surgical and clinical systems to support the entire population in a sustainable way.”
Lepard's work in Vietnam The UAB Neurosurgery Women's Leadership Council