Title:
Expectant Management versus Immediate Delivery in Women with Preeclampsia with Severe Features
Authors:
Sanjanwala Aalok R, MD, Jauk Victoria C, MPH, Cozzi GabriellaD, MD, Becker David A, MD, Harper Lorie M, MD, MCSI, Casey Brian M, MD, Tita Alan T, MD, PhD, Subramaniam A, MD, MPH1
Institutions:
1Department of Obstetrics and Gynecology and Center for Women’s Reproductive Health, University of Alabama at Birmingham, AL.
Background:
- Preeclampsia is one of the top 10 causes of pregnancy-related morbidity and mortality.
- There is evidence from small randomized trials showing that expectant management of women with severe preeclampsia can improve neonatal outcomes.
- In 2013, ACOG guidelines recommended that in select women, preeclampsia with severe features should be expectantly managed with delivery at 34 weeks’ gestation, unless indicated sooner
- The University of Alabama at Birmingham, with a >20% preeclampsia rate, widely adopted these guidelines in 2015
- There is limited data about the practical applications of these expectant management guidelines with respect to the actualized neonatal benefit and potential maternal harm
Objective:
- To compare maternal and neonatal outcomes in women with preeclampsia with severe features managed with immediate delivery versus expectant management
Study Design:
- Retrospective cohort study of women with preeclampsia with severe features delivering viable singletons at 23 – 34 weeks from January 1, 2013 – December 31, 2018 at a single tertiary care center
- Patients were excluded for:
- Multiple gestation
- IUFD at the time of diagnosis
- Delivery for other obstetrical consideration ( PPROM, labor)
- Fetal Anomalies
- Detailed chart review by two experienced reviewers was conducted.
- Primary Outcomes of the study were maternal and neonatal morbidity composites:
|
Maternal Composite Outcomes |
Neonatal Composite Outcomes |
|
Maternal ICU admission |
Suspected/confirmed sepsis |
|
Development of HELLP syndrome |
Seizures |
|
Clinically diagnosed placental abruption |
Transient Tachypnea of the newborn |
|
Pulmonary edema |
Metabolic disturbances |
|
Thrombocytopenia (platelet count < 100) |
Hyperbilirubinemia requiring treatment |
|
AKI (creatinine doubled over baseline or > 1.1) |
Mechanical ventilation |
|
Hepatotoxicity (AST > 80) |
Cardiopulmonary resuscitation |
|
Maternal stroke |
Grade III or IV intraventricular hemorrhage |
|
Death |
Necrotizing enterocolitis |
|
Respiratory distress syndrome |
|
|
Arterial cord gas pH < 7.1 |
|
|
Low APGAR score |
|
|
Hypoxic Ischemic Encephalopathy |
|
|
Neonatal Death |
- The two cohorts were defined by time from diagnosis of preeclampsia with severe features to decision for delivery
- Immediate delivery (decision for delivery < 2 days from diagnosis)
- Expectantly managed (decision or delivery > 2 days from diagnosis)
- Baseline characteristics were compared between preeclampsia management groups (immediate delivery vs. expectant management) using Students T test, Chi square, and Wilcoxon Rank sum test as appropriate
- Odds ratio with 95% confidence intervals were calculated and adjusted for covariates identified from comparison of baseline characteristics.
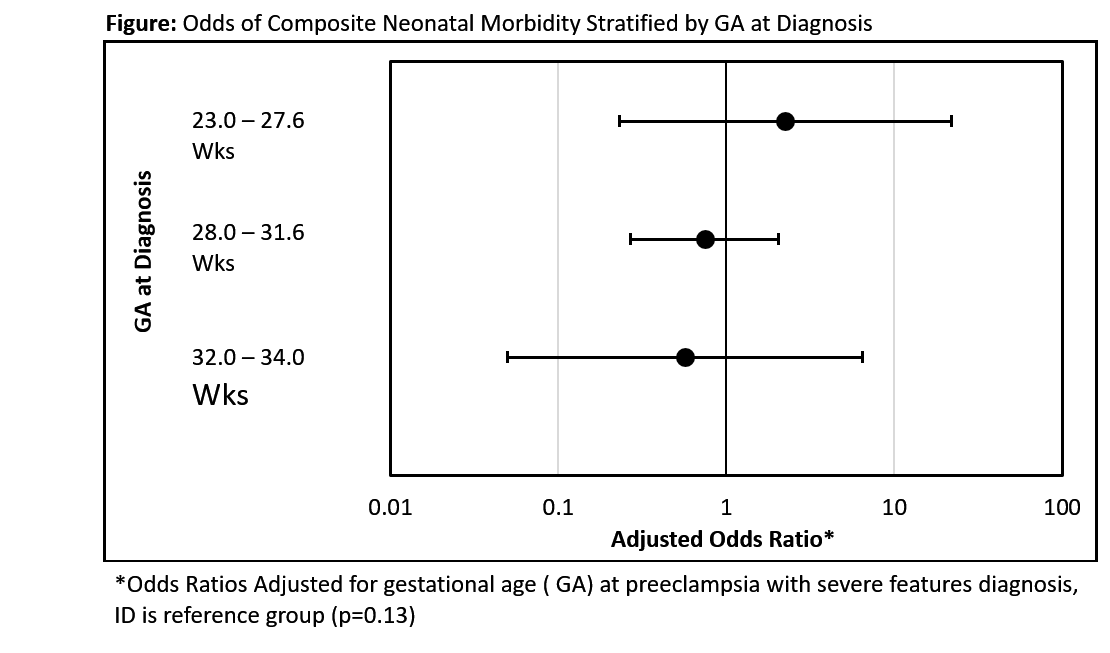
- In addition, we compared neonatal composite morbidity between immediate and expectant groups stratified by pre-defined gestation age ranges.
- Given that expectant management is often attempted by initiation/titration of oral anti-hypertensive medications, an alternate analysis was performed:
- Immediate Delivery (no initiation/titration of oral anti-hypertensives)
- Expectant management (initiation or titration of oral anti-hypertensives)
Results:
- Of 664 women with SPE, 418 met inclusion criteria.
- 122 were expectantly managed
- 296 were immediately delivered
- Baseline characteristics were balanced between groups for both expectant management and immediate delivery with the exception that the expectantly managed patients were diagnosed at an earlier GA ( Table 1)
- There was no significant difference in composite maternal morbidity (or components) between expectant management versus immediate delivery (Table 2)
- Though composite morbidity was not different, maternal hospitalization was extended by 5 days in the expectantly managed group (immediate delivery - median 6 days (IQR 5-8) vs expectant management 11 (8-19), p<0.001).
- After adjusting for age of preeclampsia with severe features diagnosis – there was reduced but non-significant reduction in neonatal composite morbidity (Table 3)
- In the alternate analysis (when expectant management was defined by oral antihypertensive use), maternal outcomes were still not compromised but neonatal outcomes significantly benefited (Tables 2 and 3)
- There were no differences in neonatal outcomes when stratified by GA range at delivery (Figure)
Conclusion:
- Expectant management of preeclampsia with severe features is associated with neonatal benefit without increased maternal harm.
- Larger studies should evaluate if these results are limited to certain GA.
|
Table 1: Baseline Characteristics for when expectant management was defined by days to delivery |
|||
|
Variable |
Immediate Delivery |
Expectant Management |
P-Value |
|
(n = 296) |
(n=122) |
||
|
Maternal Age (years) |
29.1 (6.5) |
28.8 (5.8) |
0.67 |
|
Race/Ethncity |
0.17 |
||
|
Black, non-Hispanic (%) |
173 (58.6%) |
75 (62%) |
|
|
White, non-Hispanic (%) |
105 (35.6%) |
45 (37.2%) |
|
|
Hispanic (%) |
14 (4.7%) |
1 (0.8%) |
|
|
Other (%) |
3 (1%) |
0 (0%) |
|
|
Marital Status |
0.18 |
||
|
Married (%) |
94 (32%) |
31 (25.4%) |
|
|
Other (%) |
200 (68%) |
91 (74.6%) |
|
|
Payor Status |
0.13 |
||
|
Government Assisted / Medicaid (%) |
200 (70.4%) |
75 (61.5%) |
|
|
Private Insurance (%) |
82 (28.9%) |
45 (36.9%) |
|
|
No Insurance / Self-Paid (%) |
2 (0.7%) |
2 (1.6%) |
|
|
BMI at Delivery (SD) |
36.9 (10) |
37 (8.5) |
1 |
|
Parity |
0.65 |
||
|
Nulliparous (%) |
126 (42.6%) |
49 (40.2%) |
|
|
Multiparous (%) |
170 (57.4%) |
73 (59.8%) |
|
|
Medical History |
|||
|
Smoking (%) |
49 (17.3%) |
19 (16%) |
0.75 |
|
Pre-gestational DM (%) |
25 (8.4%) |
15 (12.3%) |
0.22 |
|
Gestational DM (%) |
16 (5.4%) |
4 (3.3%) |
0.35 |
|
Chronic Hypertension (%) |
131 (44.3%) |
60 (49.2%) |
0.36 |
|
Pre-Existing Renal Disease (%) |
8 (2.7%) |
3 (2.5%) |
1 |
|
Prior Pregnancy with PIH (%) |
57 (19.3%) |
22 (18%) |
0.77 |
|
Cesarean Delivery (%) |
187 (63.2%) |
83 (68%) |
0.35 |
|
Diagnosed Fetal Growth Restriction (%) |
59 (19.9%) |
16 (13.1%) |
0.1 |
|
Hospitalization Data |
|||
|
Gestational Age at Severe Preeclamp Dx (SD) |
30.9 (2.8) |
28.5 (2.7) |
<0.001 |
|
PO Meds Started (%) |
81 (27.4%) |
82 (68.3%) |
<0.01 |
|
Admission Systolic (SD) |
166.2 (20.7) |
166.9 (19.3) |
0.76 |
|
Admission Diastolic (SD) |
98.5 (12.4) |
99 (12.4) |
0.68 |
|
Bold denotes characteristics that was identified as a covariate and accordingly adjusted for in analysis |
|||
|
Table 2: Odds Ratios for Maternal Composite Outcomes in Cohorts Defined by Days to Delivery and Oral Antihypertensive Use |
||
|
Variable |
Odds Ratio (95%CI) |
|
|
Maternal Outcomes |
EM by Days to Delivery |
EM by oral antihypertensive use |
|
Maternal Composite |
1.12 (0.58 - 2.14) |
1.42(0.77-2.6) |
|
--Maternal ICU Admission |
1.21 ( 0.11-13.52) |
-- |
|
--Development of HELLP Syndrome |
2.44(0.15-39.29) |
1.06(0.07-17.05) |
|
--Placental Abruption |
0.34(0.4-2.8) |
0.63(0.15-2.67) |
|
--Pulmonary Edema |
0.6(0.07-5.45) |
1.6(0.26-9.66) |
|
--Maternal Stroke |
-- |
-- |
|
--Eclampsia |
-- |
-- |
|
--Thrombocytopenia |
1.54(0.49 - 4.8) |
1.24(0.41-3.77) |
|
--Acute Kidney Injury > 1.1 |
3.01(0.9-10.06) |
1.88(0.54-6.53) |
|
--AST > 80 |
1.65(0.57-4.74) |
1.22(0.43-3.42) |
*EM defined by time (>2 days): ID is the reference group
**EM define by oral hypertensive use: ID is the reference group
Bold denotes significance. Omitted odds ratios indicate low incidence and inability to calculate
|
Table 3: Odds Ratios for Neonatal Composite Outcomes in Cohorts Defined by Days to Delivery and Oral Antihypertensive Use |
||
|
Variable |
Odds Ratio (95%CI) |
|
|
Neonatal Outcomes |
EM by Days to Delivery* |
EM by oral antihypertensive use** |
|
--Neonatal Composite |
0.52 ( 0.26 - 1.05) |
0.43(0.22-0.86) |
|
--Mechnical Ventilation > 24 hours |
0.45(0.2 - 1.0) |
0.41(0.19-0.9) |
|
--CPR |
0.46(0.08 -2.48) |
0.23(0.04-1.15) |
|
--Grade III or IV IVH |
0.93(0.2-4.23) |
1.04(0.21-5.2) |
|
--NEC |
0.71(0.24-2.08) |
0.92(0.31-2.7) |
|
--RDS |
0.75(0.38-1.48) |
0.8(0.44-1.47) |
|
--Arterial Cord Gas pH < 7.1 |
0.87(0.31 - 2.44) |
0.82(0.3-2.2) |
|
--5 Minute Apgar < 3 |
0.27(0.07-1.07) |
0.41(0.12-1.34) |
|
--HIE |
-- |
-- |
|
--Neonatal Death |
0.46(0.13-1.171) |
0.24(0.06-0.92) |
*EM defined by time (>2 days): Neonatal odds are adjusted for GA at diagnosis of preeclampsia with severe features; ID is the reference group/p>
**EM define by oral hypertensive use: Neonatal odds are adjusted for GA at diagnosis of preeclampsia with features and IUGR; ID is the reference group
Bold denotes significance. Omitted odds ratios indicate low incidence and inability to calculate