Title:
Effect of smoking on the development of gestational diabetes
Authors:
Timothy N Dunn MD, Yumo Xue MS, Ruby Knupp, MD, Brian M. Casey, MD, Alan N. Tita, MD, PhD, Lorie M. Harper MD MCSI
Background:
- Smoking has been associated with hyperinsulinemia and insulin resistance, and it treated as a causal risk factor for type 2 diabetes in non-pregnant adults.
- While ACOG and the ADA recommend screening patients with risk factors for pregestational diabetes or early-onset gestational diabetes (GDM) at the first prenatal visit, smoking is not listed as a risk factor.
- Current literature regarding GDM and smoking is sparse, with a mixed picture of the relationship of smoking as a risk factor for GDM.
Specific Aims:
- To determine if smoking is associated with an increased risk for GDM
Methods:
- Unplanned secondary analysis of a multi-center, randomized controlled trial that compared early to routine screening for GDM in women with a BMI ≥30kg/m2.
- Patients excluded from original trial if they had a prior cesarean delivery, pre-existing diabetes mellitus, history of bariatric surgery, major medical illnesses (such as cardiac disease or sickle cell disease among others)
- Patients included in this secondary analysis if smoking history was recorded at time of enrollment
- Primary analysis performed using dichotomous exposure of self-reported smoking, with patients reporting “yes” or “no.”
- Patients who reported smoking were stratified to those who smoked ≥10 cigarettes per day, < 10 cigarettes per day, or reported smoking formerly.
- Primary outcome was development of GDM between the exposed (smoking) and unexposed (nonsmoking) cohorts.
- Secondary outcomes included the type of GDM (A1 or A2), 50g 1-hour glucose challenge results, HbA1c levels and perinatal outcomes. Perinatal outcomes were a composite of macrosomia, primary cesarean delivery, pregnancy-induced hypertension (gestational hypertension, pre-eclampsia, or eclampsia), shoulder dystocia, neonatal hypoglycemia, or neonatal hyperbilirubinemia.
- For statistical analysis, groups were composed using chi-squared or student’s t-test for trend as appropriate. Multivariable logistic regression was used to adjust for baseline differences between groups.
Results:
- 221 (24%) of the 913 patients reported smoking.
- Smokers were less likely to be Hispanic or married, and they were more likely to report substance or alcohol use or to have chronic hypertension
- GDM incidence was similar between smoking and non-smoking groups
- After controlling for differences between groups, GDM was still not increased by smoking.
- One-hour GCT at 24 weeks was lower in smokers than nonsmokers, but both values remained below 135mg/dL.
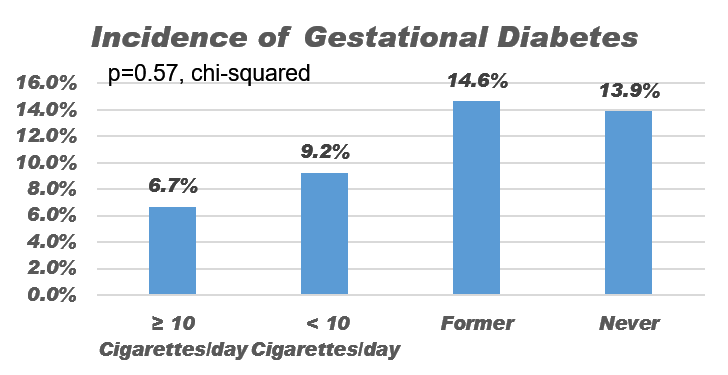
- When stratifying groups by smoking amounts, GDM and secondary outcomes remained similar between groups.
Table 1: Primary and Secondary Outcomes
|
Outcome |
Smoking N = 221 |
Non-Smoking N = 692 |
P |
|
GDM |
28 (12.7%) |
96 (13.9%) |
0.65 |
|
1-Hour GCT at 24 weeks (mg/dL) |
117.5 26.0 |
124.8 27.4 |
0.001 |
|
Composite Outcome |
122 (55.2%) |
370 (53.5%) |
0.65 |
Table 2: Outcomes stratified by smoking amount
|
Outcome |
Current ≥ 10 Cigarettes N = 15 |
Current < 10 Cigarettes N = 76 |
Former Smoker N = 123 |
Never Smoker N = 692 |
P |
|
GDM |
1 (6.7%) |
7 (9.2%) |
18 (14.6%) |
96 (13.9%) |
0.57 |
|
1-Hour GCT at 24 weeks (mg/dL) |
120.7 25.5 |
115.7 23.9 |
118.3 27.7 |
124.8 27.4 |
0.013 |
|
Composite Outcome |
8 (53.3%) |
42 (55.3%) |
68 (55.3%) |
370 (53.5%) |
0.98 |
Figure 1: Gestational Diabetes Incidence per Smoking Amount
Conclusions:
- In an obese patient population, smoking was not related to GDM development.
- There was no dose-response link between smoking and GDM.