Title:
Impact of a risk-based thromboprophylaxis protocol on postpartum bleeding and healthcare resource utilization
Authors:
Michelle Y. Lu1,2, Victoria C. Jauk2,3, Elizabeth B. Ausbeck1,2, Kacie R. Oglesby2, Rodrigo D. Muñoz Rogers2, Allison J. Lazenby2, Margaret R. Page2, Dhong-Jin Kim1,2, Brian Casey1,2, Jeff M. Szychowski1,3, Akila Subramaniam1,2
Institutions:
1Center for Women’s Reproductive Health, University of Alabama at Birmingham, Birmingham, AL
2Department of Obstetrics and Gynecology, University of Alabama at Birmingham, Birmingham, AL
3Department of Biostatistics, University of Alabama at Birmingham, AL
Background:
- Heparin-based anticoagulation for venous thromboembolism (VTE) prophylaxis in pregnant and postpartum women is not without potential risk.
- We compared measures of postpartum bleeding and resource utilization before and after adoption of a risk-based VTE prophylaxis protocol
Study Design:
- Retrospective cohort study of all deliveries at a single tertiary care center from 2013-2018
- Deliveries were categorized as pre- or post-protocol
-
- Pre-protocol deliveries:
-
-
- Delivered in 2013-2015
- No standardized VTE prophylaxis
-
-
- Post-protocol deliveries:
-
-
- Delivered in 2016-2018
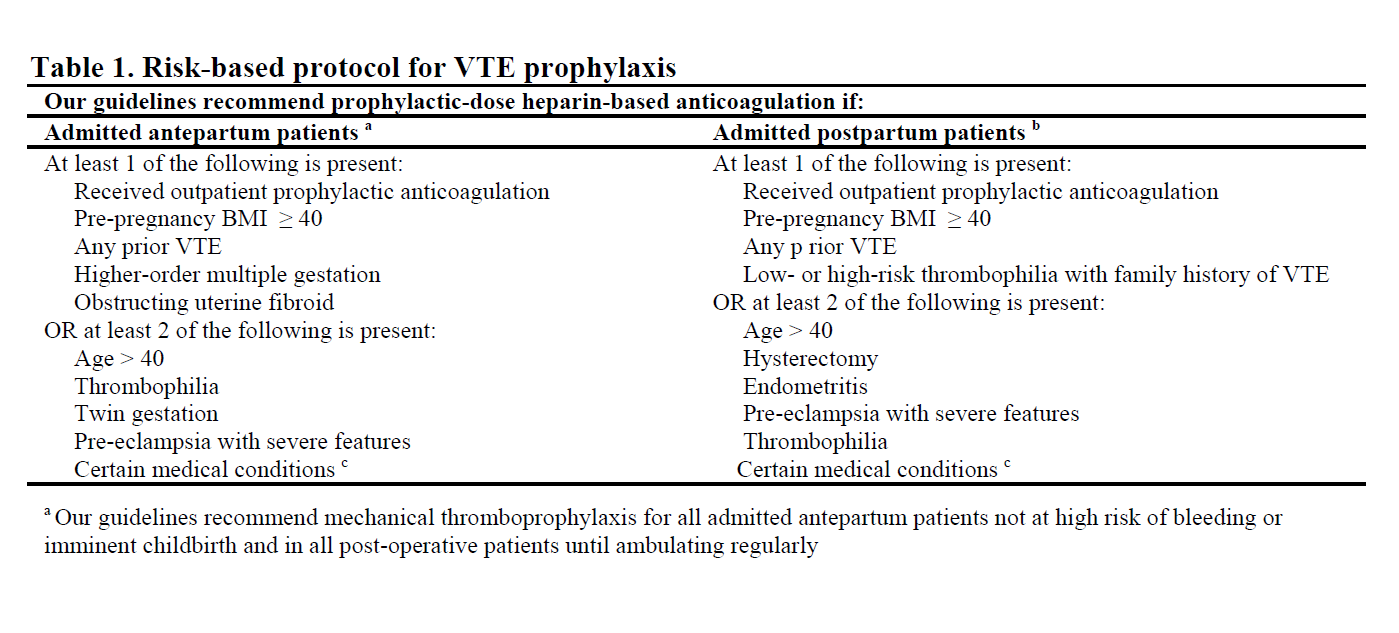
- Algorithm for anticoagulation based on antepartum/postpartum risk factors (Table 1)
-
-
- Of note, a more restrictive institutional transfusion practice was adopted in 2015
- Exclusion criteria:
-
- Patients receiving anticoagulation for active VTE or high risk of VTE
- Outcomes:
-
- Postpartum bleeding parameters
-
-
- Delivery estimated blood loss (EBL, ml)
- Receipt of uterotonics
- Receipt of packed red blood cells (pRBCs, units)
- Maximum hemoglobin change (g/dL)
-
-
- Postpartum resource utilization
-
-
- Number of hemoglobin/hematocrit studies ordered
- Patients with platelet studies evaluated
- Number of lower extremity Doppler ultrasounds obtained
- Pulmonary computed-tomography angiograms (CTA) obtained
- Maternity triage unit visits
- Number of patients readmitted
- Number of patients admitted to intensive-care units (ICU)
-
- Analysis:
-
- Outcomes were compared between pre-protocol and post-protocol cohorts
- Odds ratios (95% CIs) were calculated with the pre-protocol cohort serving as the referent group
Results:
- Of 24,232 deliveries identified, 11,799 (49%) were pre- and 12,433 (51%) were post-protocol
- Please see Table 2. We found that:
-
- Women post-protocol were 15x more likely to receive anticoagulation (16% vs. 1%, p<0.001)
- Postpartum uterotonic use was similar between groups, but more women were transfused post-protocol despite more restrictive transfusion practices
- No clinically significant differences were seen in other bleeding parameters
- There were more platelet studies ordered post-protocol but there were no changes in use of other resources detected
- Despite increased anticoagulation use, imaging studies for suspected VTEs were not different
Conclusions:
Adoption of a risk-based VTE prophylaxis protocol was associated with increased anticoagulation and blood product transfusion without a decrease in clinical evaluation of suspected VTE. Further studies to quantify if this protocol reduces VTE events or increases wound or bleeding complications are planned.