Title:
Immediate Postpartum Long-Acting Reversible Contraception in Women with Heart Disease
Authors:
Julia Maier1,2; Christina T. Blanchard, MPH1,2; Jeff M. Szychowski, PhD1,2, 3; Sara Mazzoni, MD, MPH1,2; Indranee Rajapreyar, MD4; Alexia Novara, MD5; Macie Champion, MD1,2; Alice Goepfert, MD1,2; Margaret Boozer, MD1,2; Marc Cribbs, MD4; Lorie Harper, MD, MSCI1,2; Alan Tita, MD, PhD1,2; Rachel Sinkey, MD1,2
Institutions:
- Center for Women’s Reproductive Health, University of Alabama at Birmingham, Birmingham, Alabama
- Department of Obstetrics and Gynecology, University of Alabama at Birmingham, Birmingham, Alabama
- Department of Biostatistics, University of Alabama at Birmingham, Birmingham, Alabama
- Division of Cardiovascular Disease, University of Alabama at Birmingham, Birmingham, Alabama
- Department of Obstetrics and Gynecology, Ochsner Health System, New Orleans, Louisiana
- Cardiovascular disease in pregnancy is a leading cause of maternal morbidity and mortality.
- SMFM recommends that long-acting reversible contraception (LARC) be offered to high-risk women.
- Immediate postpartum LARC (IPP LARC) allows patients reliable contraception prior to discharge from the delivery-associated hospitalization.
- Little is known about IPP LARC in women with cardiovascular disease.
- To compare postpartum contraception in women with heart disease before and after implementation of an immediate postpartum LARC (IPP LARC) program.
- Observational cohort of women with cardiac disease managed by the UAB Comprehensive Pregnancy & Heart Program
- Delivery at UAB between 3/1/2015 – 6/30/2019
- Pre-implementation (Pre) group:
-
- Delivery before IPP LARC implementation (3/1/2015 – 1/31/2017)
- Post-implementation (Post) group:
-
- Delivery after IPP LARC implementation (2/1/2017 – 6/30/2019)
- Primary outcome
-
- LARC (intrauterine device (IUD) or etonogestrel implant) use postpartum (PP), defined as IPP LARC or LARC at PP visit.
- Secondary outcomes
-
- Contraception intent at delivery
- IPP IUD expulsion rate
- Results
-
- 159 women were included, 63 (40%) were Pre, 96 (60%) were Post
- Baseline characteristic were similar between groups.
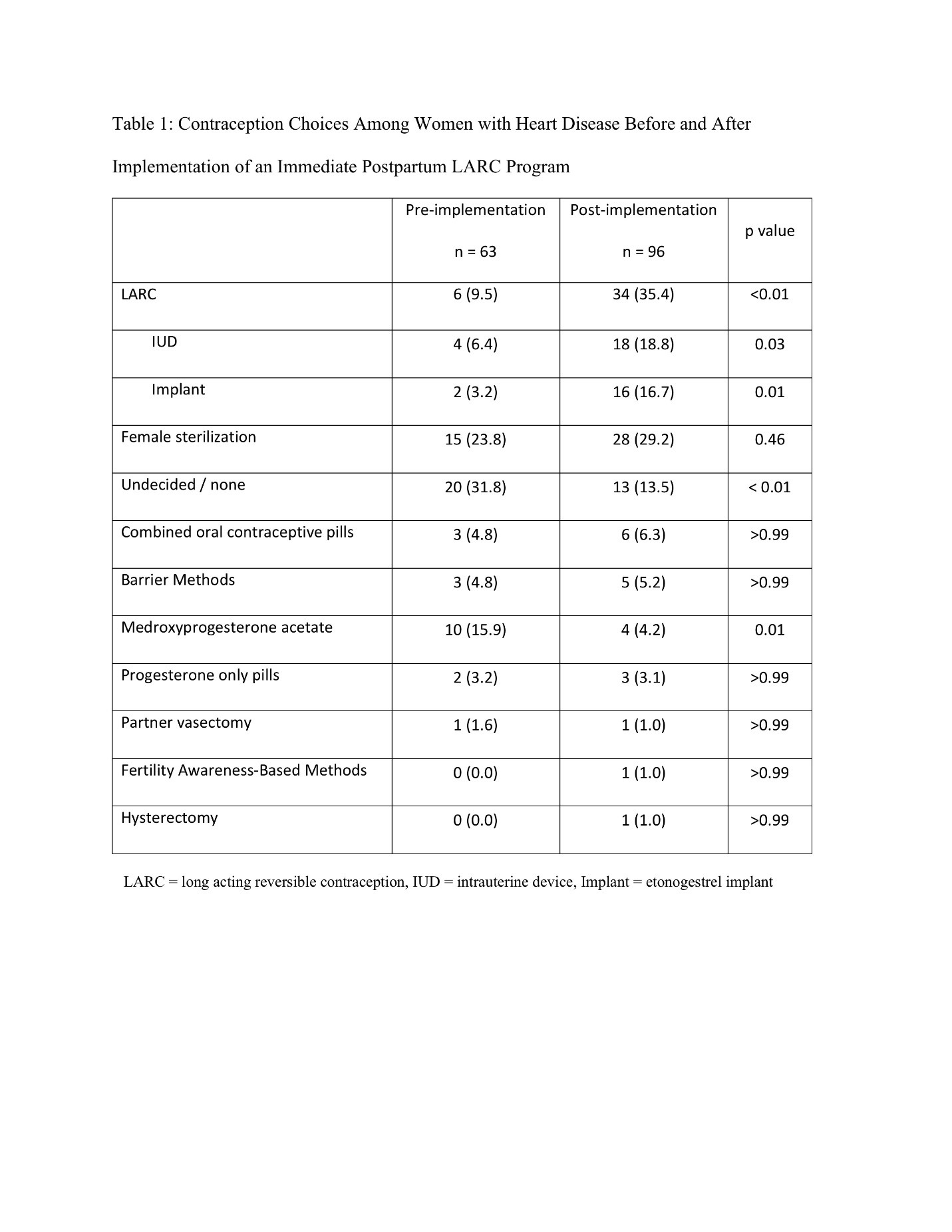
- Total LARC use tripled after IPP LARC implementation, 10% vs 35%, p < 0.01, despite similar LARC intent at delivery: 33% vs 43%, p=0.21.
- Rates of women without contraception plans at delivery decreased from 32% to 14%, p < 0.01
- Medroxyprogesterone acetate use decreased: 16% vs 4%, p=0.01.
- Female sterilization rates remained similar before and after IPP LARC implementation: 24% and 29%, p = 0.46.
- PP visit rates were similar between Pre and Post groups: 70% and 72%, p=0.78
- 1 IPP IUD expulsion occurred.
- LARC use in women with heart disease tripled after implementing IPP LARC.
- LARC is the most effective way to prevent unintended pregnancies; thus, IPP LARC should be a public health priority for women with heart disease to reduce their disproportionate burden of maternal morbidity and mortality.