Title:
Effect of intramuscular progesterone on the cervicovaginal microbiome in high-risk women with midtrimester cervical shortening
Authors:
Akila Subramaniam, MD, MPH, Boyi Guo, MS, Elena Lobashevsky, MD, PhD, William van der Pol, MS, Elliot Lefkowitz, PhD, Casey Morrow, PhD, Jeff Szychowski, PhD, Nengjun Yi, PhD, John Owen, MD, MSPH.
Background:
- Intramuscular 17-hydroxyprogesterone caproate (17-OHP) is widely used to decrease preterm birth (PTB) in women with prior spontaneous PTB (SPTB, high-risk).
- Yet, its mechanisms of action and effects on the cervicovaginal (CV) microbiome are unknown.
- Furthermore, 17-OHP has been shown to be more beneficial in some populations compared to others.
Objective:
- We sought to compare the CV microbiome in high-risk women with midtrimester CL shortening who did versus did not receive 17-OHP.
Study Design:
- We performed a nested cohort study using stored CV biospecimens collected in a multicenter randomized trial of ultrasound-indicated cerclage for shortened CL <25mm in women with a prior SPTB at 160/7 – 226/7 weeks.
- In the parent trial, 17-OHP use was documented.
- In this current study, we used CV specimens collected at a follow-up CL scan <25mm (i.e. women with normal initial CL and a follow-up CL <25mm) to allow for an effect from 17-OHP use.
- DNA was extracted and a V4 amplicon library prepared and sequenced on the MiSeq platform.
- The QIIME package, using DADA2, generated Amplicon Sequence Variants with a high yield of species-level identifications.
- Microbiome composition and group comparisons (17-OHP vs no 17-OHP) were assessed through relative taxon abundance and alpha and beta diversity.
- Negative binomial models, adjusting for cerclage placement, were used in taxa-specific analysis
- False discovery rate was used to adjust for inflated type I error.
Results:
- 128 samples were analyzed
- 36 with 17-OHP use
- 92 without 17-OHP use
- Overall, 67 of 128 participants (52%) received a cerclage.
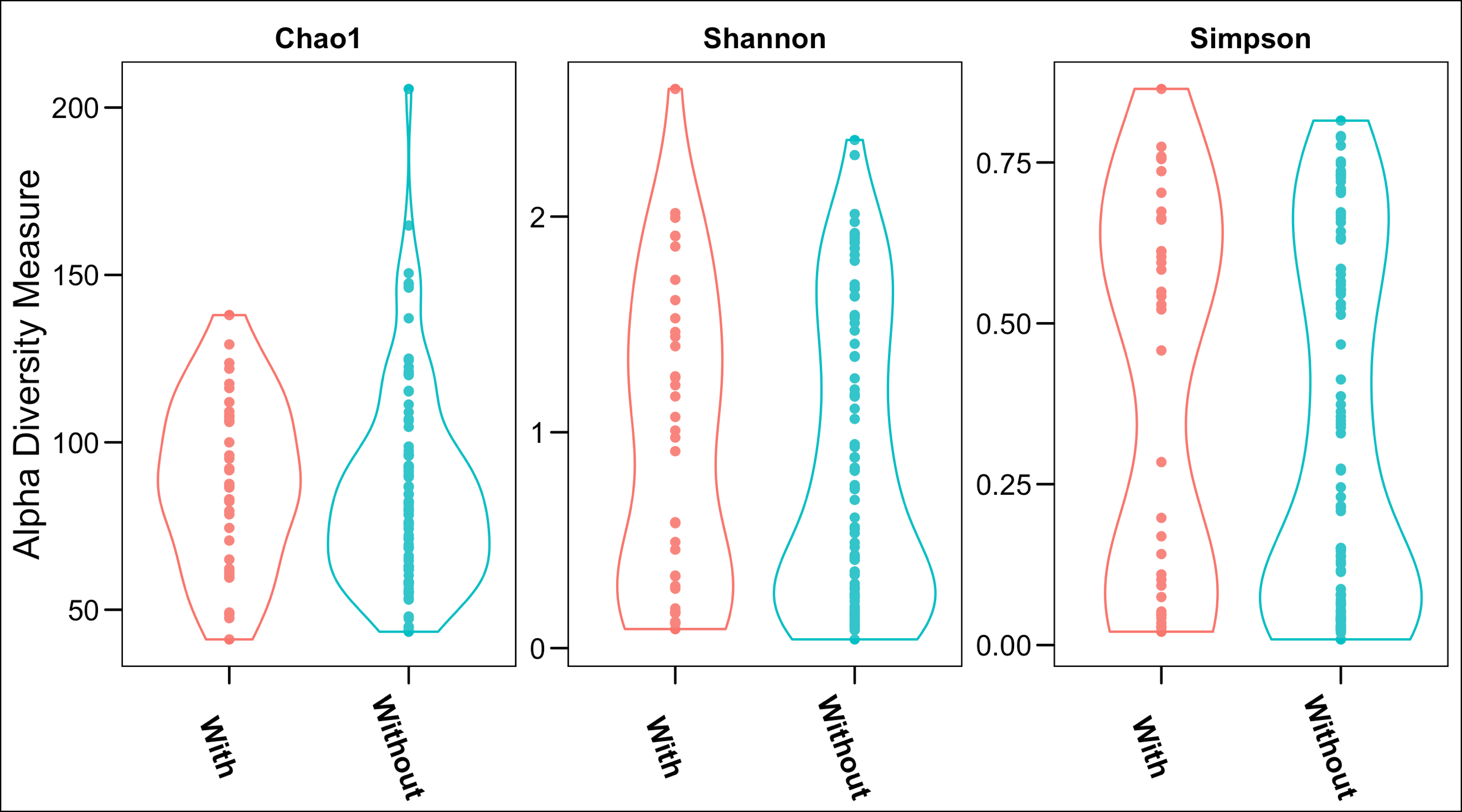
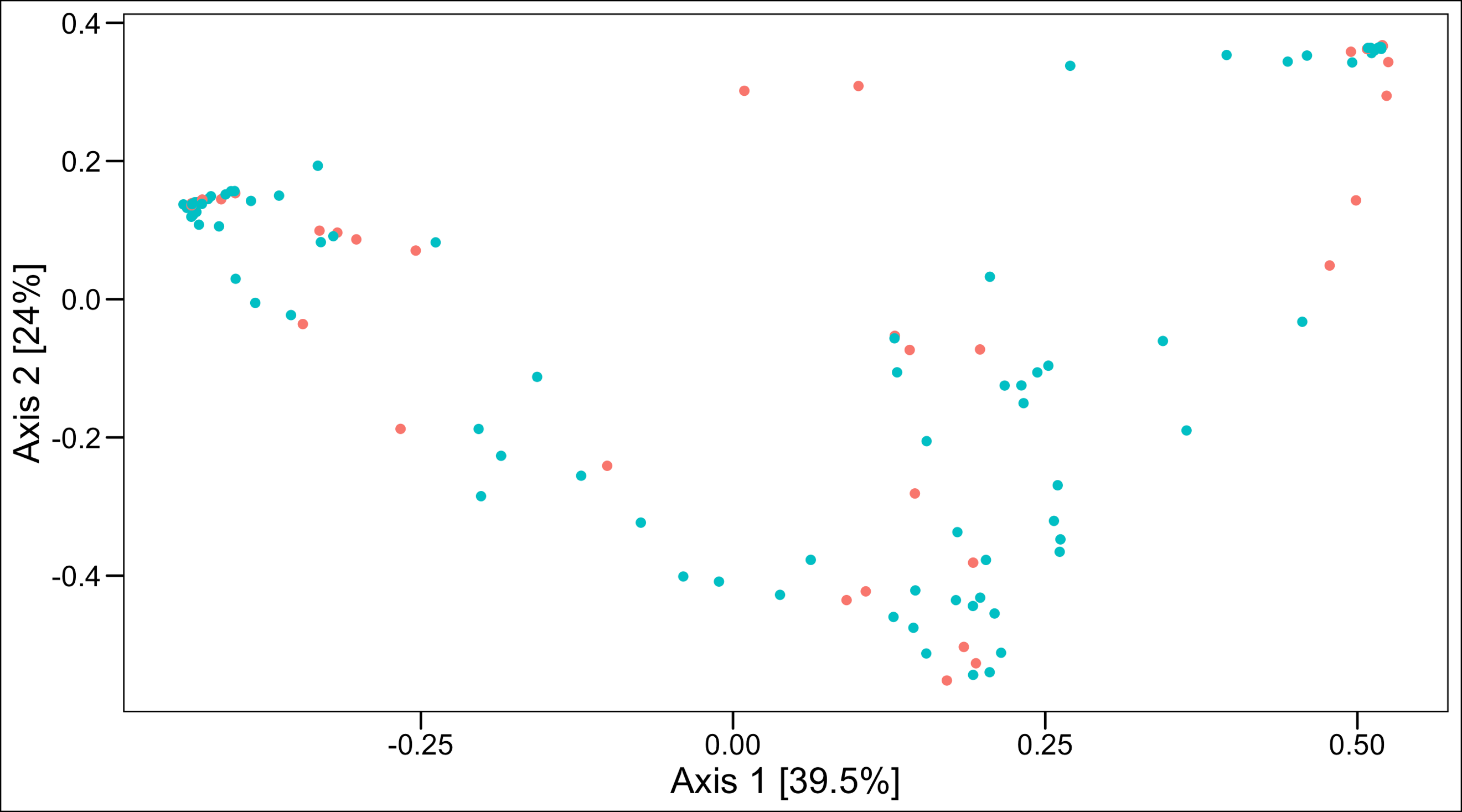
- There were no significant differences in alpha diversity (Figure 1a) or beta diversity between the groups (Figure 1b, PERMANOVA p = 0.3)
- However, 17-OHP use was significantly associated, even after adjustments, with
- Decreased abundances of Moraxellaceae Acinetobacter (FDR p=0.003)
- Decreased abundances of Prevotellaceae Prevotella (FDR p=0.02)
- Increased Lactobacillus iners (FDR p=0.02)
Conclusion:
- 17-OHP use is associated with decreased abundances of two known inflammatory pathogens
- 17-OHP use is also associated with increased L. iners – a pro- or anti-inflammatory pathogen depending on host response.
- This effect of 17-OHP should be further explored to determine its association with the unpredictable response to 17-OHP in certain populations.
Figure 1. Comparison of alpha diversity (a. top panel) and beta diversity (b. bottom panel – Principal Coordinate Analysis) between women with a prior SPTB with or without 17-OHP use