Title:
Mid-trimester cervical length screening: effect of poorly-developed lower uterine segment on pregnancy outcome
Authors:
David A. Becker MD, Timothy N. Dunn MD, Jeff M. Szychowski PhD, John Owen MD, MSH for the Center for Women’s Reproductive Health and Department of Obstetrics and Gynecology, University of Alabama at Birmingham
Background:
- Poorly-developed lower segment (PDLUS), or cervical isthmus, is characterized by a long “cervix” (> ~5 cm), S-shaped canal, different echogenicties in the “cervix”, increased bladder-to-amniotic cavity distance, and “internal os” cephalad to the inferior edge of the bladder reflection (Figure 1).
- PDLUS precludes accurate cervical length (CL) measurement as the location of the true internal os is obscured.
- PDLUS is protective against spontaneous preterm birth (sPTB) in women with a prior sPTB < 34 weeks.
Objectives:
- To identify whether PDLUS affects duration of gestation in low-risk women.
Study Design:
- Retrospective cohort study of singleton gestations in women with no history of sPTB who underwent universal CL screening between 1/2016-8/2018 at UAB.
- Exclusion criteria: any progesterone exposure, fetal anomalies
- Women with a measured (Normal) CL ≥ 25mm were compared to those with PDLUS.
- Primary outcome: gestational age (GA) at birth
- A sample of 1135 with a 4:1 Normal:PDLUS ratio had 80% power to detect a 1/2 week difference in birth GA (ɑ=.05, GA SD=2.4 weeks).
- Secondary outcomes: sPTB < 37 weeks, preterm labor (PTL) evaluation
- A Cox survival model considered time from CL scan to delivery.
- Indicated PTB were censored at birth.
- Time was censored at 39 weeks to account for elective induction.
Results:
- 990 (79%) women with Normal CL and 265 (21%) women with PDLUS were included (Table).
- Birth GA was 38.7 ± 2.4 weeks with Normal CL vs 38.9 ± 2.0 weeks with PDLUS (p=0.10).
- The incidence of sPTB < 37 weeks was 3.6% for Normal CL and 1.1% for PDLUS (p=0.04).
- 19% with Normal CL had at least 1 PTL evaluation vs. 17% with PDLUS (p=0.54).
- In the Cox model, PDLUS was found to have a significantly lower hazard ratio (HR) of 0.67 (95% CI 0.46, 0.98; p=0.04) for earlier birth.
- After controlling for parity, the HR fell to 0.64 (p=0.02) (Figure 3).
Conclusions:
- PDLUS observed at mid-trimester CL screening in low-risk women was associated with a significantly lower rate of sPTB < 37 weeks and a lower HR for earlier birth.
- There was no difference in GA at birth between Normal CL and PDLUS.
Figure 1. Poorly-developed lower uterine segment.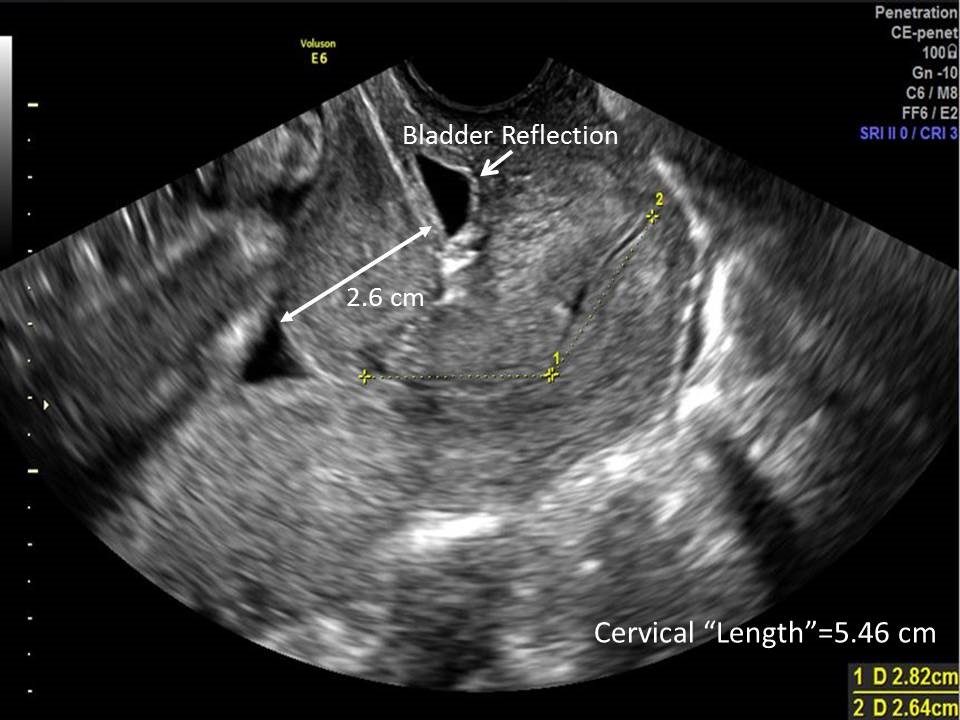
Figure 2. Measured normal cervical length.
Figure 3. Cox survival model of time from cervical length measurement to delivery.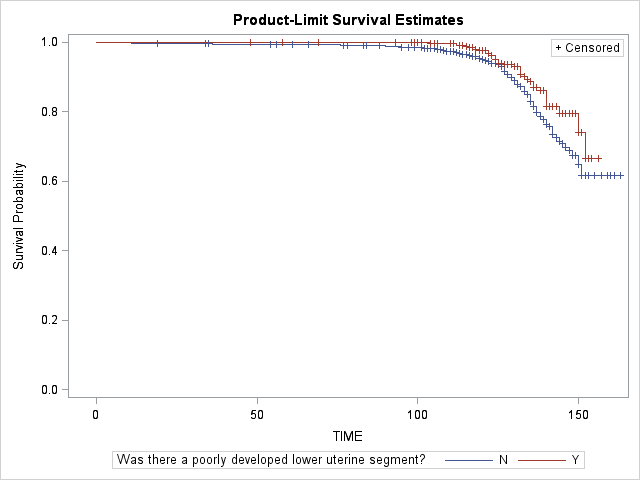
Table. Demographics
|
Characteristic |
Normal CL (n=990) |
PDLUS (n=265) |
p-value |
|
GA @ CL measurement |
19.4 ± 1.1 |
19.4 ± 1.1 |
0.89 |
|
Age |
26 ± 5.5 |
27 ± 5.6 |
0.03 |
|
Race White Black Hispanic Asian Unknown |
12% 49% 17% 1% 0% |
11% 61% 6% 1% 1% |
0.30 |
|
BMI (kg/m2) |
29 ± 8.0 |
31 ± 8.6 |
0.009 |
|
Tobacco use |
21% |
16% |
0.27 |
|
Substance abuse |
13% |
9.5% |
0.29 |
|
Multiparous |
60% |
68% |
0.01 |
|
STI |
20% |
16% |
0.18 |
|
Chronic HTN |
7.8% |
6.8% |
0.59 |
|
Diabetes mellitus |
10% |
11% |
0.79 |
*Data presented as mean ± SD or percentage.