Title:
Are rates of spontaneous preterm birth stable across a range of normal cervical lengths?
Authors:
Timothy N. Dunn MD, David A. Becker MD, Jeff M. Szychowski PhD, John Owen MD, MSH for the Center for Women’s Reproductive Health and Department of Obstetrics and Gynecology, University of Alabama at Birmingham
Background:
- Cervical length screening is an effective adjunct to reducing recurrent spontaneous preterm birth (sPTB) in high-risk women, but the efficacy of universal screening in women with no prior sPTB is uncertain.
- In high-risk women, a range of normal cervical lengths (CL) (≥25) has been associated with a stable risk of recurrent sPTB.
- It is unclear how rates of sPTB vary over a range of measured-normal CLs in low-risk women.
Objectives:
- To identify the risk of sPTB in low-risk women according to range of normal CLs.
Study Design:
- Retrospective cohort study of singleton gestations in women with no history of sPTB who underwent universal CL screening between 1/2016-8/2018 at UAB.
- Inclusion criteria: measured CL of ≥25mm (i.e. in the normal range).
- Exclusion criteria: any progesterone exposure, fetal anomalies, and unmeasurable CL due to a poorly-developed lower uterine segment (cervical isthmus).
- Interval CL groups of 25-29mm, 30-34mm, 35-39mm, 30-44mm, and ≥45mm (χ2 test of trend) and CL as a continuum (logistic regression and ROC curve) were considered.
- Primary outcome: sPTB <37 weeks.
- Secondary outcome: number of hospital evaluations for suspected preterm labor (PTL).
Results:
- 990 low-risk women were identified for study inclusion (Table 1).
- Mean CL was 39.2±6.0 mm (interdecile range=31.6, 47.0) measured at 19.4±1.1 weeks.
- The cohort incidence of sPTB <37 weeks was 3.6%.
- Mean GA at delivery was 38±2.4 weeks.
- There was a significantly decreasing trend in sPTB across increasing CL (p=0.004, Table 2).
- Increasing CL as a continuous variable was associated with lower odds of sPTB (OR=0.92, 95% CI 0.87, 0.98).
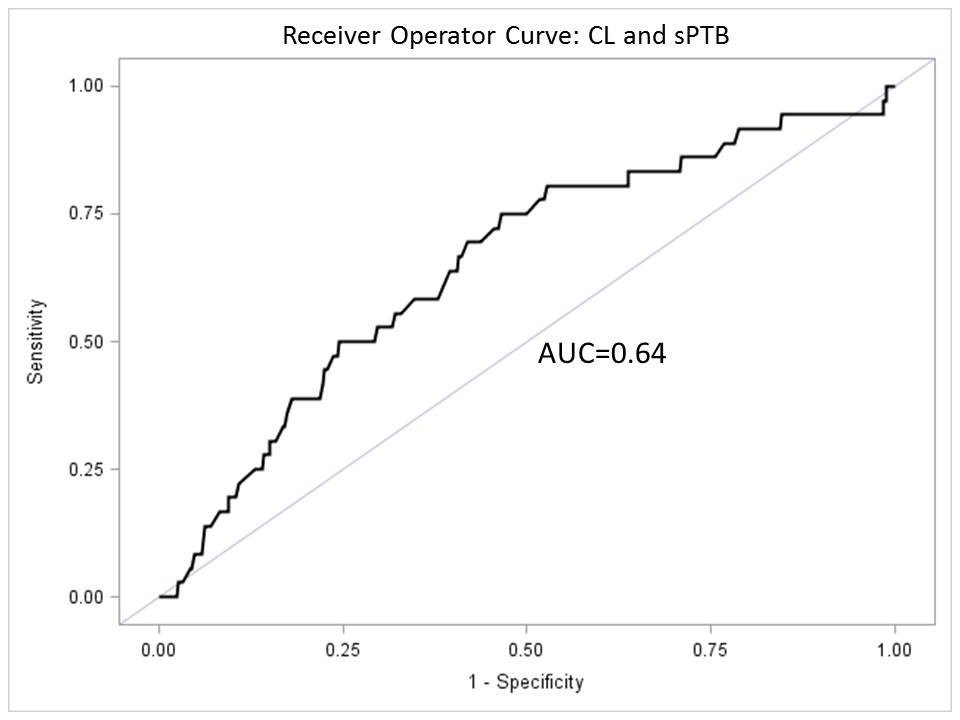
- ROC (Figure) AUC for sPTB was only 0.64.
- Median number of hospital evaluations for PTL was 0 (range 0-4), and the number of evaluations for suspected PTL was not associated with CL (p=0.259).
Conclusions:
- Among low-risk women with a normal CL, increasing CL was associated with decreased risk of sPTB, though only with modest effect.
- Normal CL ranges appear to be a poor predictor of sPTB in low-risk women.
- Increasing CL was not associated with number of hospital evaluations for PTL.
|
Characteristic |
25-29mm N=32 |
30-34mm N=223 |
35-39mm N=297 |
40-44mm N=237 |
≥45mm N=201 |
p-value |
|
Age |
27 ± 5 |
25 ± 5 |
26 ± 5 |
27 ± 6 |
26 ± 5 |
0.001 |
|
BMI (kg/m2) |
25 ± 5 |
29 ± 8 |
29 ± 8 |
29 ± 8 |
30 ± 8 |
0.031 |
|
Multiparous |
56% |
51% |
59% |
68% |
61% |
0.004 |
|
Prior Cesarean |
6% |
16% |
15% |
18% |
17% |
0.478 |
|
GA @ CL measurement |
19.5 ± 1.0 |
19.4 ± 1.0 |
19.4 ± 1.1 |
19.3 ± 1.0 |
19.4 ± 1.1 |
0.892 |
Table 2. Primary and secondary outcomes.
|
Outcome |
25-29mm N=32 |
30-34mm N=223 |
35-39mm N=297 |
40-44mm N=237 |
≥45mm N=201 |
p-value |
|
Spontaneous PTB <37 weeks |
3.1% |
7.6% |
3.7% |
1.7% |
1.5% |
0.004 |
|
Hospital evaluations |
0.2 ± 0.5 |
0.2 ± 0.6 |
0.3 ± 0.7 |
0.2 ± 0.5 |
0.2 ± 0.6 |
0.259 |
Figure