To diagnose MS, three major criteria must be satisfied:
- Evidence of MS damage in at least 2 distinct locations within the central nervous system
- Evidence that MS-like damage has occurred on at least two separate points in time
- Other diseases which may mimic or resemble MS must be ruled out with appropriate laboratory or other investigations
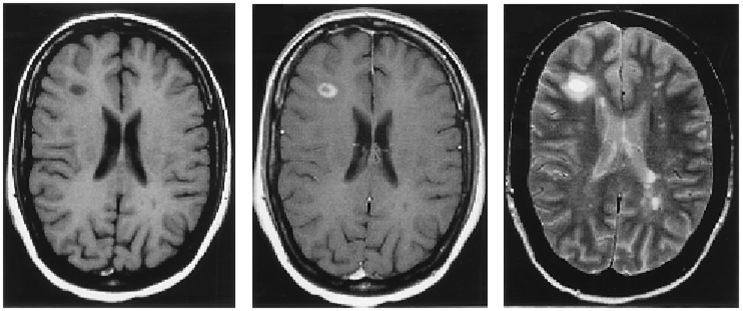
The tool which has become most useful at visualizing the damage caused by MS is the MRI scanner. The MRI provides the physician with detailed pictures of the brain and spinal cord, including the lesions caused by MS inflammation. The MRI can, in some instances, also tell the physician if the lesions have recently formed or if they have been present for some time.
 The MRI scanner has vastly shortened the time it now takes to make an MS diagnosis. Before the invention of MRI, patients would have to experience two or more attacks before a diagnosis could be made. With MRI, many patients are diagnosed after their first relapse, and MRI is used to satisfy the other diagnostic criteria. This has led to earlier diagnosis and initiation of disease modifying treatment for many MS patients.
The MRI scanner has vastly shortened the time it now takes to make an MS diagnosis. Before the invention of MRI, patients would have to experience two or more attacks before a diagnosis could be made. With MRI, many patients are diagnosed after their first relapse, and MRI is used to satisfy the other diagnostic criteria. This has led to earlier diagnosis and initiation of disease modifying treatment for many MS patients. MRI is painless, noninvasive, and does not expose the body to radiation. It is often used in conjunction with the contrast agent gadolinium, which helps distinguish new plaques from old. However, since these lesions can also occur in several other neurological disorders, they are not absolute evidence of MS.
Other tests that may be used to diagnosis MS include visual evoked potentials (VEP) and studies of cerebrospinal fluid (the colorless liquid that circulates around the brain and spinal cord). VEP tests measure the speed of the brain's response to visual stimuli. VEPs can sometimes detect lesions missed on MRI, and VEPs are particularly useful when abnormalities seen on MRI do not fully satisfy the criteria for MS. Like imaging technologies, VEP is helpful but not conclusive because it cannot identify the cause of lesions, only establish that they are there.
Examination of cerebrospinal fluid can show cellular and chemical abnormalities often associated with MS. These abnormalities include increased numbers of white blood cells and higher-than-average amounts of protein, especially myelin basic protein and an antibody called immunoglobulin G. Physicians can use several different laboratory techniques to separate and measure the various proteins in MS patients' cerebrospinal fluid. This process often identifies the presence of a characteristic pattern called oligoclonal bands.
A number of other diseases may produce symptoms similar to those seen in MS. Other conditions with an intermittent course and MS-like lesions of the brain's white matter include polyarteritis, lupus erythematosus, syringomyelia, tropical spastic paraparesis, some cancers, and certain tumors that compress the brainstem or spinal cord. Progressive multifocal leukoencephalopathy can mimic the acute stage of an MS attack. Physicians may also consider stroke, neurosyphilis, spinocerebellar ataxias, pernicious anemia, diabetes, Sjogren's disease, and vitamin B12 deficiency, depending on the patient. Recent reports suggest that the neurological problems associated with Lyme disease may present a clinical picture much like MS.
While it can still be difficult for the physician to differentiate between an MS attack and symptoms that can follow a viral infection or even an immunization, our growing understanding of disease mechanisms and the expanded use of MRI is enabling physicians to diagnose MS with more confidence than ever before. Today, most patients who undergo a diagnostic evaluation for MS will be classified as either having MS or not having MS. However, there are still cases where a person may have the clinical symptoms of MS but not meet all the criteria. In these cases, a diagnosis of "possible MS" is used.
Investigators are continuing their search for a definitive test for MS. Research using MRI has yielded several new imaging approaches which may detect the disease earlier and in greater detail than can be done with current standard imaging methods. While these techniques are not yet in use in a widespread basis, in the future they may become commonplace in clinical practice.
While standard MRI provides an anatomical picture of lesions, magnetic resonance spectroscopy (MRS) yields information about the brain's biochemistry; specifically, it can measure the brain chemical N-acetyl aspartate. Decreased levels of this chemical can indicate nerve damage.
Magnetization transfer imaging (MTI) is able to detect white matter abnormalities before lesions can be seen on standard MRI scans by calculating the amount of "free" water in tissues. Demyelinated tissues and damaged nerves show increased levels of free (versus "bound") water particles.
Diffusion-tensor magnetic resonance imaging (DT-MRI or DTI) measures the random motion of water molecules. Individual water molecules are constantly in motion, colliding with each other at extremely high speeds. This causes them to spread out, or diffuse. DT-MRI maps this diffusion to produce intricate, three-dimensional images indicating the size and location of demyelinated areas of the brain. Changes in this process can then be measured and correlated with disease progression.
Functional MRI (fMRI) uses radio waves and a strong magnetic field to measures the correlation between physical changes in the brain (such as blood flow) and mental functioning during the performance of cognitive tasks.
In addition to helping scientists and physicians better understand how MS develops-an important first step in devising new treatments-these approaches offer earlier diagnosis and enhance efforts to monitor disease progression and the effects of treatment.