Media contact: Beena Thannickal
You can find them from the banks of the Mississippi River in Bolivar County, Mississippi, to the red-brick walls of Tuskegee University, 350 miles away in Alabama’s Macon County.
"We all have a name,” says Claudia Hardy, MPA, director of Community Outreach in the O’Neal Comprehensive Cancer Center at UAB. “All of us have been labeled the ‘cancer lady’ in our communities.”
For the past 20 years, Hardy has developed the Cancer Center’s Deep South Network for Cancer Control, helping to train more than 1,200 laypeople to spread lifesaving information, and hope, in their neighborhoods and hometowns. Adapting a model originally designed to tackle conditions such as teen pregnancy and hypertension, Hardy and the Deep South Network are addressing the cancers that are particularly prevalent in rural and urban minority communities in the South: breast, cervical and colon cancer. And new partnerships are expanding the Deep South Network’s successful model into lung cancer.
 For 20 years, Claudia Hardy has built connections with "natural helpers" in communities across Alabama and Mississippi. The Community Health Advisors (CHAs) "are really trusted individuals, men and women of integrity that people turn to," Hardy says.
For 20 years, Claudia Hardy has built connections with "natural helpers" in communities across Alabama and Mississippi. The Community Health Advisors (CHAs) "are really trusted individuals, men and women of integrity that people turn to," Hardy says.
Taking on lung cancer
Grants from the National Cancer Institute supporting the Deep South Network ended in 2016, but funding from the Cancer Center and the Alabama Department of Public Health has allowed the program to maintain a presence in eight counties. Now, working in partnership with the Lung Cancer Alliance, the Cancer Center and its successful Deep South Network community health advisor (CHA) model are taking on the leading cancer killer of men and women in Alabama and the United States. The Alabama Lung Cancer Awareness, Screening and Education (ALCASE) program, funded by a three-year grant from the Bristol-Myers Squibb Foundation, will begin recruiting and training up to 150 CHAs in a seven-county program area in February 2019. “We are recruiting men and women of all races and backgrounds over the age of 19 to join us in these efforts,” Hardy says.
Join the fight: learn more about becoming a Community Health AdvisorAlthough lung cancer screening can find the disease early, when the possibility of a cure is highest, only 4 percent of individuals in the United States are screened each year. “We hope using the successful CHA model will help improve screening rates among these at-risk individuals,” says Michael J. Birrer, M.D., Ph.D., director of the O’Neal Comprehensive Cancer Center at UAB. “There is a great lack of awareness about the potential benefits of screenings and, for many, a reluctance to engage in the screening process.”
| When the Deep South Network was formed in 1999, African American women in the Black Belt were 17 percent less likely than white women in the region to have regular mammograms. By the end of the program, the pattern had been dramatically altered. “In the Medicare population, more blacks were getting screened than whites,” Hardy says. |
Community gatekeepers prove value
CHAs have proven their value at combatting lack of awareness and reluctance. When the Deep South Network was formed in 1999, African American women in the Black Belt were 17 percent less likely than white women in the region to have regular mammograms. By the end of the program, the pattern had been dramatically altered. “In the Medicare population, more blacks were getting screened than whites,” Hardy says.
The CHAs “are gatekeepers — really trusted individuals, men and women of integrity that people turn to,” Hardy explains. “They are natural helpers who build trust. They take the information and put it into their own words.” In addition to explaining the risks of cancer and the benefits of early detection through screening, the CHAs “also stay informed on how the systems operate,” Hardy adds. In Alabama, for instance, state law means low-income women diagnosed with breast cancer are automatically enrolled in Medicaid and fully treated, while with cervical cancer “it’s a case-by-case basis,” Hardy says, “but we’ve been able to build relationships with doctors across the state to take care of these patients.”
 CHAs provide education, but they do much more besides, including helping overcome the biggest barrier to cancer screening: fear. "They sit with people until they get their results," Hardy says. "They hold their hands. They’re never off the clock."
CHAs provide education, but they do much more besides, including helping overcome the biggest barrier to cancer screening: fear. "They sit with people until they get their results," Hardy says. "They hold their hands. They’re never off the clock."
Reaching the “total person”
Hardy, who earned her undergraduate degree at UAB in 1992 and later a master’s degree in public administration, grew up in the Black Belt, in rural Dallas County. “I have lived in both the rural and urban worlds,” she says. “I understand the poverty, the culture, the language.”
The barriers are real, Hardy says. “Some people just don’t know — they are the easiest to move,” she explains. Many Black Belt residents have jobs that make it hard to take time off to be screened or have no transportation to get to appointments. “There is no Uber in rural areas,” Hardy says. “You’re at the mercy of other people. If you don’t have a car, you may have to pay someone $25 or $35 to take you into town.” The biggest obstacle, however, is fear, Hardy says. “They are afraid of what they may find out.”
That’s where the CHAs shine. “They sit with people until they get their results,” Hardy says. “They hold their hands. They’re never off the clock; they’ll take calls at all hours.” Over the years, successful CHAs have come from all education levels and backgrounds, Hardy notes. “The common thread is they are people with passion. They are truly involved because they want to improve the health of their communities.”
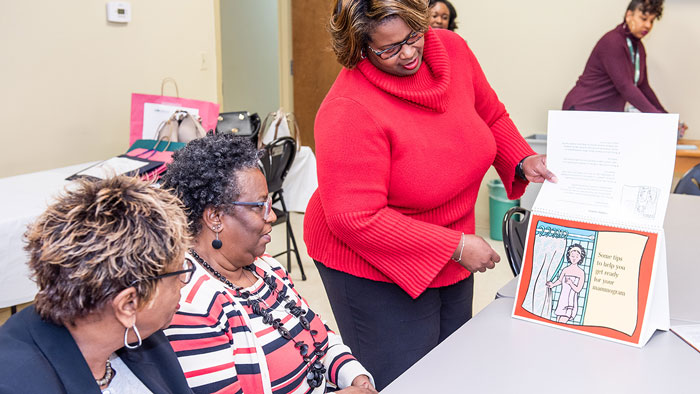
 A study by Monica Baskin (standing) showed that CHAs could implement a weight-loss program that produced clinically meaningful weight loss in a significant proportion of participants.
A study by Monica Baskin (standing) showed that CHAs could implement a weight-loss program that produced clinically meaningful weight loss in a significant proportion of participants.
Community-based participatory research
The Deep South Network was designed to be a true partnership between communities and researchers. One need that CHAs and other community members noted again and again was the obesity crisis. The prevalence of obesity in African American women is more than 1 in 2. “We can do cancer screening, but we also have to reach the whole person,” Hardy says. UAB researchers developed and tested a number of innovative programs to promote exercise and healthy eating in these communities. In a partnership with UAB’s Minority Health and Health Disparities Research Center, the Deep South Network recruited more than 1,800 people to “neighborhood walking teams,” with a retention rate greater than 50 percent. The Body and Soul Initiative, geared toward African-American churches, focused on the importance of eating a healthy diet. Both programs implemented cancer prevention strategies.
| "When poverty, hopelessness and despair are all around, we can motivate people to know they have options. We can contribute to turn midnight into day." |
Several years ago, the CHAs helped implement a truly randomized trial of a weight-loss program aimed at African-American women, with UAB’s Monica Baskin, Ph.D., a professor in the School of Medicine Division of Preventive Medicine and associate director for Community Outreach and Engagement at the Cancer Center, as principal investigator. “Women strongly influence meal decisions in the household, so we thought it was important to focus on them,” Hardy says. The study demonstrated that trained laypeople were able to make a difference. In a paper in the Journal of Internal Medicine, published in 2017, the researchers noted that more than a quarter of participants lost at least 5 percent of their body weight, with significant reductions in blood pressure, waist circumference and triglycerides. The CHAs “were able to deliver a translation of a high-intensity behavioral intervention… resulting in clinically meaningful weight loss and improvement in other metabolic outcomes in a significant proportion of participants,” the authors noted.
Other research has explored the importance of social support in maintaining healthy eating and exercise, the impact of depression and stress on weight loss and even contrasted the different gut microbes present in African American and white women, which could help explain disparities in rates of colorectal cancer.
The work of the Deep South Network and its CHAs has touched more than 124,000 people. That continues to motivate Hardy. “There’s more work to be done,” she says. “When poverty, hopelessness and despair are all around, we can motivate people to know they have options. We can contribute to turn midnight into day.”
To learn more about becoming a Community Health Advisor, contact Claudia Hardy at (205) 975-5454 or chardy@uab.edu.