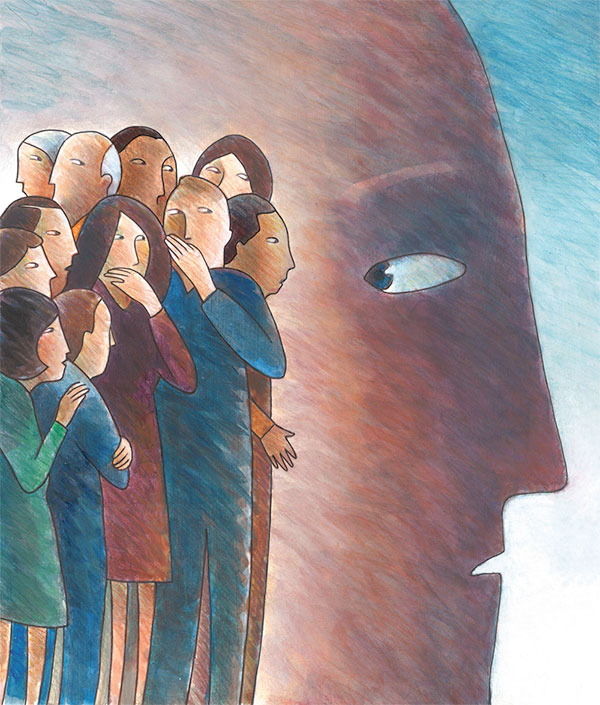
 Illustration by Ernie EldredgeInvestigators from the University of Alabama at Birmingham have developed a new conceptual framework highlighting how unique dimensions of individual-level HIV-related stigma might affect the health of those living with HIV. According to the paper’s authors, little is known about the mechanisms through which stigma leads to worse health behaviors or outcomes.
Illustration by Ernie EldredgeInvestigators from the University of Alabama at Birmingham have developed a new conceptual framework highlighting how unique dimensions of individual-level HIV-related stigma might affect the health of those living with HIV. According to the paper’s authors, little is known about the mechanisms through which stigma leads to worse health behaviors or outcomes.
The framework, published in the American Journal of Public Health, looks at perceived community stigma, experienced stigma, internalized stigma and anticipated stigma as barriers to both HIV prevention and engagement in care. An intersectional framework looks at how multiple social statuses intersect at an individual level, such as HIV status, race, gender or sexual orientation, and a broader level, such as structural stigmas in society including racism, sexism, HIV-related stigma and classism, to produce health inequalities.
The conceptual framework suggests that individual-level dimensions of HIV-related stigma operate through interpersonal factors, mental health, psychological resources and biological stress pathways.
“Those living with HIV often fight fear and experiences of HIV-related stigma, affecting their quality of life and mental health, as well as engaging poorly in their HIV care and treatment,” said Janet Turan, Ph.D., professor in the UAB School of Public Health Department of Health Care Organization and Policy. “Our proposed conceptual framework for individual-level dimensions of stigma and potential individual and interpersonal mechanisms explains how stigma affects each individual’s HIV-related health.”
HIV-infected individuals may be judged by others to be in marginalized social groups, causing social stress because of their minority social position, which could lead to important implications for their health.
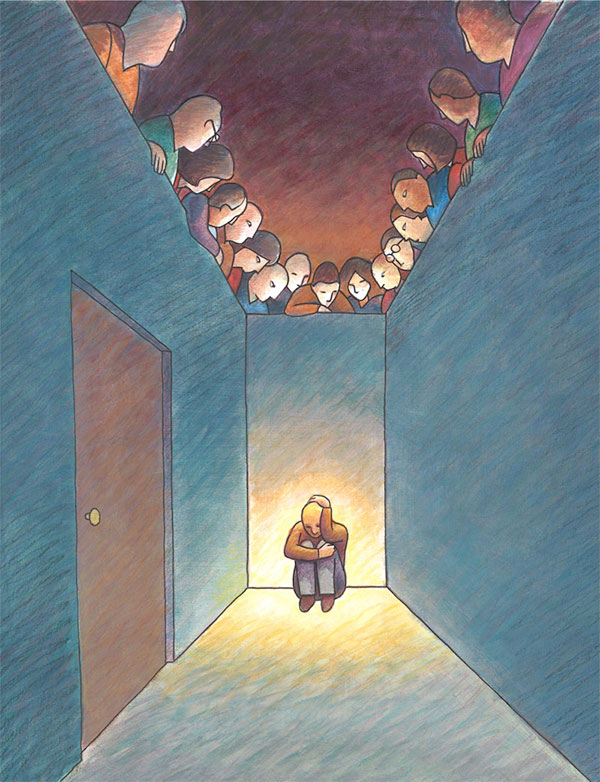 Illustration by Ernie Eldredge“People living with HIV may be stigmatized by their partner, family members and members of the community,” said Bulent Turan, assistant professor in the UAB College of Arts and Sciences Department of Psychology. “Those who are close to the individual and who place them in a minority status may cause more harm to their overall mental and physical health. In fact, health care workers who stigmatize people living with HIV can be detrimental to treatment outcomes.”
Illustration by Ernie Eldredge“People living with HIV may be stigmatized by their partner, family members and members of the community,” said Bulent Turan, assistant professor in the UAB College of Arts and Sciences Department of Psychology. “Those who are close to the individual and who place them in a minority status may cause more harm to their overall mental and physical health. In fact, health care workers who stigmatize people living with HIV can be detrimental to treatment outcomes.”
People living with HIV may have a lack of physician trust, poor adherence to care and lower quality of life if stigmatized by those involved in their care. They may experience social stress in various ways, including externally by discrimination of others, anticipation of discrimination by others, internalizing negative attitudes from those around them and/or hiding their sexual orientation. Each of these can adversely affect health behaviors, physical health, and outcomes such as depression, adherence to care and HIV health outcomes.
According to the study, stigma can worsen HIV-related health both directly through physiology and indirectly through engagement in care behaviors. The framework suggests that stigma at a structural level may also affect individuals living with HIV directly or through individualized-level dimensions, such as internalized stigma, and individual-level mechanisms, such as depression.
The conceptual framework encompasses recent advances in stigma science that can inform future research and interventions aiming to address stigma as a driver of HIV-related health.
“By targeting appropriate coping behaviors and mechanisms associated with HIV stigma, future policy and programs can be better developed to reduce stigma and provide a healthy life for those living with HIV,” Turan said.