 November is National Hospice and Palliative Care Month, recognizing specialized care that helps relieve not only physical pain, but also the emotional, social and spiritual suffering associated with serious illness. The goal of palliative care is to achieve the best possible quality of life for patients and their families affected by life-altering medical conditions.
November is National Hospice and Palliative Care Month, recognizing specialized care that helps relieve not only physical pain, but also the emotional, social and spiritual suffering associated with serious illness. The goal of palliative care is to achieve the best possible quality of life for patients and their families affected by life-altering medical conditions.
University of Alabama at Birmingham’s Center for Palliative and Supportive Care pursues this goal with interdisciplinary teams that deliver care to older adults and patients with advanced or life-threatening illnesses, as well as survivorship care and dignified end-of-life care. UAB makes palliative care services available for both inpatients and outpatients, depending on the patient’s circumstances and preferences.
“The phrase we often use is ‘an extra layer of care,’” said Rodney Tucker, M.D., director of the UAB Center for Palliative and Supportive Care. “By that we mean an extra dimension of support for a broad spectrum of patients with serious conditions such as heart failure, dementia, cancer, lung transplant and others. As an interdisciplinary team, we try to address all the domains of suffering: physical, psychosocial, emotional and spiritual, because clinical data indicate that when you address a whole person, you consistently get better outcomes. This personalized care helps patients tolerate other treatments better, and with cancer patients, for example, they may even live longer if they receive good palliative care alongside chemotherapy.”
Along with compassionate, personalized treatment, the palliative care teams strive for innovation. The program plans to implement telehealth resources by the end of 2018, with the goal of scaling UAB Medicine’s palliative care expertise to a broader population of patients throughout the Southeast.
“I think this is the most exciting next phase of palliative care,” Tucker said. “We will have the ability to provide virtual consults, which will be a tremendous benefit for patients who are not mobile or who may live a great distance from the hospital. That also benefits patients’ families, and caring for their needs and relieving some of the burdens is part of our mission. If a nurse or caregiver can take the technology to a patient’s residence, then our staff at The Kirklin Clinic, for example, can conduct a virtual visit. That should be available from us at some point in 2018. In the very near future, we may be delivering some aspects of palliative care to a large number of outpatients that way.”
In many respects, Tucker sees palliative care as a return to a previous medical culture that focused on better and broader communication between doctor and patient.
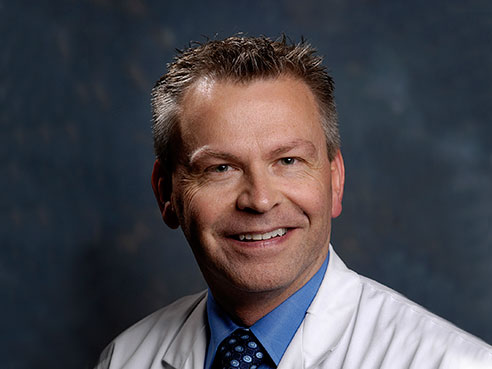 Rodney Tucker, M.D., director of the UAB Center for Palliative and Supportive Care“After the antibiotic era, we basically changed what people die from,” Tucker said. “They used to die from infectious diseases. Now we see patients dying from diseases of lifestyle: heart disease, stroke, cancer. During this transition, we sometimes lost the art of thinking of patients as whole people, or talking with them about their health beyond the confines of a condition they might have. In hospital settings, they became ‘the gallbladder in room 204’ or ‘the heart attack in 718.’ Now we focus on communication with the patient and family. We talk about a patient’s goals. Rather than waiting to die, they can determine, with our assistance, how they wish to live this set of circumstances. We ask them what they want this journey to look like. Through these many facets of palliative care and better communication, we hope to return the art of medicine to the science of healing.”
Rodney Tucker, M.D., director of the UAB Center for Palliative and Supportive Care“After the antibiotic era, we basically changed what people die from,” Tucker said. “They used to die from infectious diseases. Now we see patients dying from diseases of lifestyle: heart disease, stroke, cancer. During this transition, we sometimes lost the art of thinking of patients as whole people, or talking with them about their health beyond the confines of a condition they might have. In hospital settings, they became ‘the gallbladder in room 204’ or ‘the heart attack in 718.’ Now we focus on communication with the patient and family. We talk about a patient’s goals. Rather than waiting to die, they can determine, with our assistance, how they wish to live this set of circumstances. We ask them what they want this journey to look like. Through these many facets of palliative care and better communication, we hope to return the art of medicine to the science of healing.”
Recent studies show that, among a growing number of health care professionals, there is an emphasis on providing more and earlier access to palliative care. Clinicians have seen that this care can mitigate the toll taken by extreme treatments administered to cancer patients, for example, in the wider effort to consistently achieve better outcomes. Awareness has exponentially expanded in the health care realm. Tucker notes that UAB Medicine plays a big role in “spreading the good word about palliative care.”
“Our UAB Medicine mission is three-part: advance knowledge through research, offer excellent clinical care, and educate, which we do a lot of,” Tucker said. “But there’s a fourth component of our mission in palliative care, and that’s to change the culture in our community – to change how people think about a serious illness. We are very fortunate at UAB and throughout the Birmingham community to have the Palliative Care program that includes clinical programs at UAB, the Birmingham VA, and Children’s of Alabama, not just for the care provided, but also because of the training.”
UAB has scheduled Palliative Care Leadership Center training sessions for Huntsville Hospital and Baptist Health in Montgomery, because they are both starting to look closely at their palliative care programs.
“We’re making an impact on the culture of health care in our region and across the nation and also influencing policy, because we are spreading the word about palliative care to areas that may not be as rich in resources as we are at this academic center,” Tucker said.