In 2017, more than 107,000 new cases of gynecologic cancers were diagnosed in American women. Of those, an estimated 31,600 women lost their fight with a gynecologic cancer.
However, many women are unaware of their potential risk for developing a gynecologic cancer and the symptoms that indicate they may have cancer.
What is gynecologic cancer?
According to the Centers for Disease Control and Prevention, gynecologic cancer is any cancer that starts in a woman’s reproductive organs. The five primary gynecological cancers include ovarian, cervical, vulvar, uterine/endometrial, and vaginal, all posing unique symptoms and risk factors.
 “Most people who get a gynecologic cancer don’t have obvious risk factors,” said Warner K. Huh, M.D., division director of the University of Alabama at Birmingham Division of Gynecologic Oncology. “With these types of cancers, what women can control is being screened regularly and seeking medical advice if something doesn’t seem right with their bodies.”
“Most people who get a gynecologic cancer don’t have obvious risk factors,” said Warner K. Huh, M.D., division director of the University of Alabama at Birmingham Division of Gynecologic Oncology. “With these types of cancers, what women can control is being screened regularly and seeking medical advice if something doesn’t seem right with their bodies.”
Any woman can be at risk for any gynecologic cancer. Risk tends to increase with age, and there is always a heightened possibility of cancer due to family history or race. Lifestyle choices such as chronic smoking and obesity can impact one’s risk for developing a gynecologic cancer; for instance, there is a correlation between higher rates of uterine/endometrial cancers in obese women.
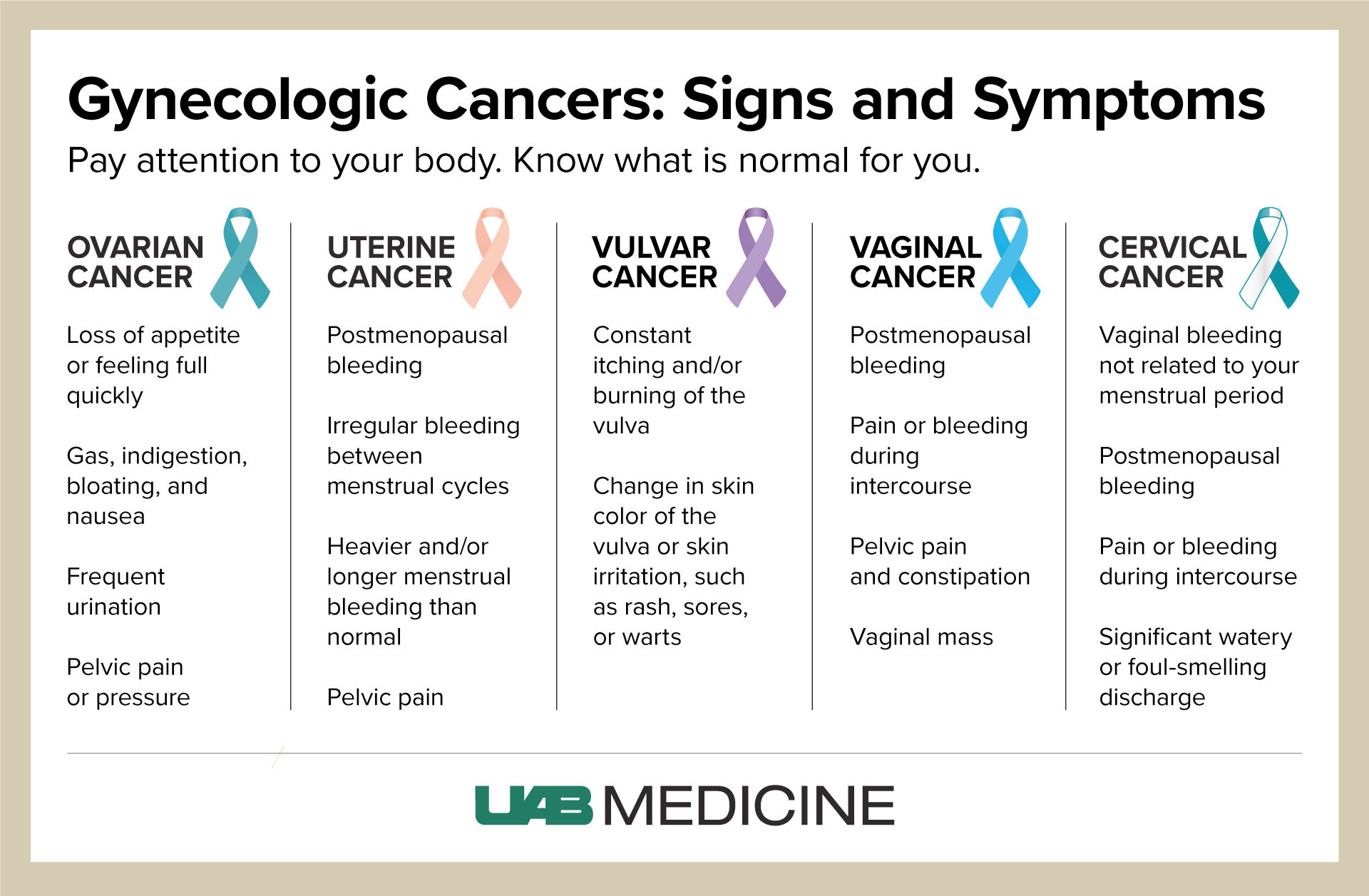
Signs and symptoms
A primary challenge in the detection of gynecologic cancers is that many of the signs and symptoms are ones that women experience regularly, be they with menstruation or as side effects from another condition. Furthermore, symptoms range from woman to woman, so it can be hard to definitively say that each woman will experience the same thing.
“What women need to be looking for is the chronicity and abnormal frequency of symptoms, even if the symptoms are ones that don’t seem out of the ordinary,” said Huh, who is also the senior medical officer for the cancer service line at the UAB Comprehensive Cancer Center. “If they are experiencing symptoms like persistent bloating, ongoing bleeding or persistent pelvic pain, they need to be aware of the persistence and length of these symptoms as they may indicate that a formal medical evaluation is needed.”
While each woman’s reaction may be different, the signs and symptoms below are general indicators for each cancer. As Huh notes, it is important for women to use these symptoms as guides, ultimately knowing that they are the only ones who know for certain that there is something atypical, uncomfortable or intolerable about the symptoms they are experiencing.
- Cervical: vaginal bleeding unrelated to one’s period; postmenopausal bleeding; pain or bleeding during intercourse; significant or foul-smelling discharge
- Ovarian: loss of appetite or feeling full quickly; gas; bloating; nausea; frequent urination; pelvic pain or pressure
- Uterine/Endometrial: postmenopausal bleeding; irregular bleeding between menstrual cycles; heavier and/or longer menstrual bleeding; pelvic pain
- Vaginal: postmenopausal bleeding; pain or bleeding during intercourse; pelvic pain and constipation; vaginal mass
- Vulvar: constant itching and/or burning sensation in the vulva (outer part of female genitals); change in skin color of the vulva, including rashes, sores or warts
Prevention and detection
Women undergo different screenings at their annual OBGYN appointment — screenings that can ultimately save their lives if they are positive for cancer. Both the Pap test and HPV test are routinely administered at an OBGYN visit and are conducted during pelvic exams by means of cell collection with a swab.
The Pap test — often referred to as a Pap smear — tests for cervical cancer through the collection of cells from the cervix. The test not only can detect active cancerous cells but can detect changes that may identify a risk for cancer in the future. The Pap test does not screen for cancers beyond cervical. Women as young as 21 will undergo routine Pap tests in their annual OBGYN visit, and their doctor may suggest a schedule for Pap tests moving forward, such as getting one every three years.
The HPV test is similar to the Pap test in the way cells are collected, but it tests more broadly for other types of cancers and human papillomavirus. The current recommendation is that women 30 years and older receive an HPV test in addition to the Pap test at their annual visit.
“We know that, with most malignancies, screening is critical and early detection can help save the life of the woman,” Huh said. “The biggest takeaway for women is to stay mindful of their bodies, report any symptoms that appear even remotely irregular and make sure they have their screenings conducted on a yearly basis. These actions can ultimately save their life.”
What about the HPV vaccine?
Huh strongly advises that all women — and men — receive the vaccine to protect against cancers caused by human papillomavirus. The recommendation is for girls and boys starting as young as age 9 up until age 26 to receive the required dosages. In women, the HPV infection can cause cervical, vaginal and vulvar cancers, so the vaccine provides added protection for this population.
If you or a woman you know is experiencing abnormal symptoms, talk to your doctor about what you are feeling. Pay attention to your body and know what is or is not normal for you.