Faculty from every department in the UAB School of Health Professions presented abstracts at the 2023 Association of Schools Advancing Health Professions (ASAHP) Annual Conference. A dozen faculty representing each of our five departments delivered seven abstracts.
The ASAHP was chartered in September 1967 as a non-profit for academics and others concerned with higher education in allied health. Our dean, Andrew Butler, is a current member of the ASAHP board of directors.
The conference also marked the graduation of Brenda Bertrand, Ph.D., RDN, program director, UAB M.S. in Nutrition Sciences, from the ASAHP Leadership Development program. Bertrand, who was the first faculty member from UAB to be chosen by ASAHP for this program, presented “Identifying Best Practices for Faculty Mentoring in Health Professions” with other members of the ASAHP leadership class.
“Identifying Best Practices for Faculty Mentoring in Health Professions”
Brenda Bertrand (Department of Nutrition Sciences); James Onate (The Ohio State University); Paul Anderson (New York Institute of Technology); Jessica Stahulak (University of Arkansas for Medical Sciences); Jon Williamson (University of Texas Southwestern Medical Center)
 Onate, Bertrand, Stahulak, Butler
Onate, Bertrand, Stahulak, Butler
ISSUE: Practices and programs of mentorship for health professions faculty vary considerably across disciplines, departments, and schools, and it remains unclear what are key elements and best practices for faculty mentoring.
METHOD: This project used a mixed methods approach to identify best practices for faculty mentoring. A qualitative design was used identify key themes about effective faculty mentoring from semi-structured interviews with 10 faculty mentoring experts across 5 academic health professions institutions. A quantitative design was used to identify common characteristics from faculty mentoring programs across selected institutional members of ASAHP.
OUTCOME: Results will be presented about practical recommendations for contextual faculty mentoring and for faculty mentoring programs for academic health professionals.
CONCLUSION: Development of faculty mentoring programs varies widely across ASAHP institutions with most involved in professional development at the institutional level as opposed to division/departmental level. Future evaluation of faculty mentorship program development at the division/department level warrants consideration for improving retention rates and work-life balance satisfaction.
“Photo Journaling While Studying Abroad: Cultivating Cultural Humility”
Rachel Ashcraft and Jewell Dickson (Department of Occupational Therapy)
 Dickson-Clayton, Butler, Ashcraft
Dickson-Clayton, Butler, Ashcraft
Cultural humility is a necessary skill for all healthcare workers to create a healthcare workforce that is truly diverse, equitable, and inclusive. It is not always clear how cultural humility is instilled within healthcare professional students. To address this issue, an occupational therapy study abroad program with an emphasis on building cultural humility skills was designed and implemented. The ability to self-reflect as well as remain respectfully curious about learning about other cultures are both key to the development of cultural humility. A study abroad program to South Africa was designed with an emphasis on ongoing self-reflection and building respectful curiosity. Reflective photo journaling was utilized as a teaching method to support student development of cultural humility throughout the experience. Outcomes of this experience positively indicated that use of reflective photo journaling when paired with an intentional study abroad experience can support the development of cultural humility. Cultural humility is something that is continually cultivated throughout one’s professional life. This experience was effective at laying a foundation for cultural humility that students can build on for years to come.
“The Impact of Psychological Safety in Ambulatory Interprofessional Teams”
Tera Webb (Department of Clinical and Diagnostic Sciences) and Michelle Brown (Department of Health Services Administration)
 Webb, Butler
Webb, Butler
AIM: Favorable patient care delivery is more likely in healthcare environments that are perceived as psychologically safe. The aim of this study is to determine the impact of psychological safety in ambulatory interprofessional (IP) teams.
METHOD: This was a cross-sectional study with quantitative and qualitative survey data. Variables measured: psychological safety (PS), transactive memory systems (TMS), and quality of care. Psychometric analyses were performed and acceptable. Path analysis performed for hypothesis testing. Results: The dataset included 209 individuals that were aggregated into 27 teams. Over 20 clinic specialties represented. Professions represented: medical doctors, advanced practice providers (PA/NP), nurses, technicians/technologists, assistants, administrative, and other staff. PS was positively associated with TMS and perceived quality of care.
CONCLUSION: First, this study reinforces previous evidence in the literature that states PS positively impacts quality of care. Secondly, findings demonstrate that PS leads to the emergence of TMS. When TMS emerges, professionals are more likely to share specialized knowledge across the teams.
“Promoting Interprofessional Competencies Using a Critical Care Simlulation”
Michelle Brown and Erin Blanchard (Department of Health Services Administration); Cody Black and Tera Webb (Department of Clinical and Diagnostic Sciences); Penni Watts (School of Nursing)
Interprofessional (IP) education is an excellent way to introduce students to team-based healthcare delivery. We designed an IP intensive care unit simulation that was grounded in experiential learning theory and the Healthcare Simulation Standards of Best Practice. We developed a multi-modal extendedtime, 5 patient ICU simulation and included students in Medical Laboratory Science (MLS), Accelerated Masters in Nursing Pathway (AMNP), and Physician Assistant Studies (PA). The intent of the simulation was to challenge learners with significant complexity to allow for critical thinking, prioritization, and team-based communication challenges. The simulation included a prebrief, scenarios with objectives that were mutually constructed with all professions, and a tiered, structured debrief. The tiered debriefing occurred on three levels: in the room to unpack the scenario, a full-group debrief simulation to discuss teamwork and communication and managing critical patients, and a discipline-specific debrief to clarify any concerns related to their field.
“Teamwork STAT! The Use of IP Acute Care Simulation to Facilitate Collaborative Practice”
Valley McCurry (Department of Occupational Therapy); Tara Pearce (Department of Physical Therapy)
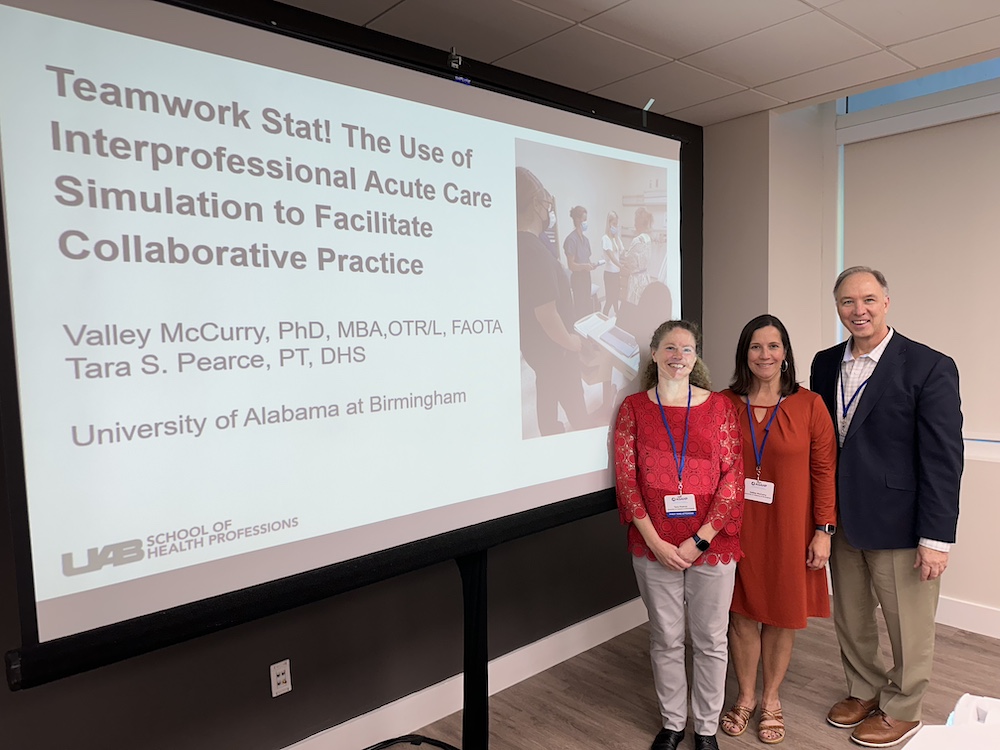 Pearce, McCurry, Butler
Pearce, McCurry, Butler
Many students in health profession programs report a lack of exposure to providing services in an acute care hospital setting, leading to feelings of anxiousness, diminished interest, and lower self-efficacy. We created and piloted a high-fidelity simulation-based learning activity that included students in both OT and PT programs. First-year students were exposed to the acute care environment as either standardized patients or embedded participants. Teams of second year students were tasked with completing initial Concurrent Presentation Abstracts 2023 ASAHP Annual Conference Wednesday, October 18 35 evaluations, interventions, discharge planning, and documentation for simulated patients in multiple units of an acute care hospital setting by engaging in interprofessional practice, then participated a formal debrief of the cases. All students completed the Acute Care Confidence Survey and the Readiness for Interprofessional Learning Scale pre and post to determine if participation in the SBLA increased their confidence in their knowledge, skills, and behaviors, and their confidence in working as a member of an interprofessional team. Students were also asked to reflect on their own strengths, areas in which they can improve, and possible integration of this experience into future fieldwork or clinical education.
“An Interprofessional Education Model Through a Service-Learning Platform"
Wei Li and Muhammad Maqbool (Department of Clinical and Diagnostic Sciences); Bradley Jenkins (School of Public Health); and Leslie Hemby and Nandini Vobbilisetty (students, Department of Clinical and Diagnostic Sciences)
ISSUE: To establish an interprofessional education model through a service-learning platform.
METHOD: Students/trainees from different professions collaborate to deliver free healthcare services to a local homeless population under the supervision of faculty members. The participating programs include Biomedical Sciences, Medical Laboratory Sciences (MLS), Nutrition and Dietetics (ND), Occupational Therapy (OT), Physician Assistant (PA), Physical Therapy (PT), and Social Work (SW).
OUTCOME: SW students are responsible for arranging the sign-ups as well as guiding the homeless participants to different stations. MLS students run a finger-stick test for measuring blood glucose, lipid profile as well as HbA1c. PA students take a medical history and vital signs and give a focused physical examination. PT and OT students give corresponding tests and treatments based on the needs of the homeless participants. ND, OT, and PT students also provide educational services to the underserved group.
CONCLUSION: A service-learning platform is effective not only for providing services to the underserved population but also for students to be trained in an interprofessional mode.
“A Virtual Interprofessional Experience Between School of Health Professions and School of Medicine”
Lizzy Davis and Brenda Bertrand (Department of Nutrition Sciences); Caroline Harada (Heersink School of Medicine)
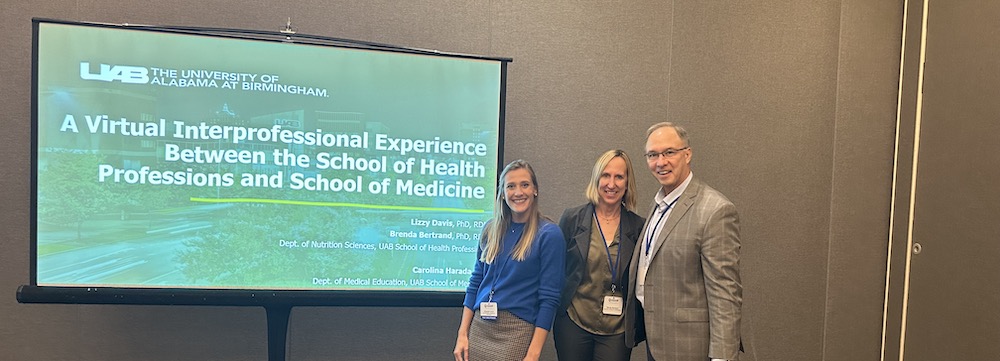 Davis, Bertrand, Butler
Davis, Bertrand, Butler
ISSUE: Online education is rapidly increasing, creating barriers to high quality interprofessional training for health profession students.
METHOD: Students from Schools of Health Professions (Dietetic Interns, DI) and Medicine (Medical Students, MS) worked together as DI-MS dyads to complete a virtual program to train MS to provide nutrition coaching for patients with pre-diabetes from a single outpatient clinic that provides healthcare services to uninsured patients. The project required MS to interview DI on how to counsel adult patients with pre-diabetes. Then, MS provided nutrition coaching to DI who role-played patients. Lastly, MS performed nutrition coaching sessions with real patients. De-brief notes and written reflections were coded and analyzed using thematic qualitative analysis.
OUTCOME: Twenty-four DI trained 30 MS to complete nutrition coaching with 31 patients at the outpatient clinic, adding up to $3100 labor cost. Common themes that emerged included reduced intimidation experience by DI from the medical role and increased perceived value by DI.
CONCLUSION: Virtual experiences between School of Health Professions and Medical Schools is advantageous by teaching interprofessional skills and applied to service-learning.

