Case History
28 year-old male with inguinal lymphadenopathy. IHC shows many CD15-, CD30+ large cells. CD20+ and CD3+ large cells seen. Background lymphocytes mostly T-cells with inverted CD4/CD8 ratio. Ki-67 elevated throughout infiltrate. EBER shows scattered + cells.
- EBV+ classic Hodgkin lymphoma
- Acute EBV infection (infectious mononucleosis)
- EBV+ PTCL
- EBV+ DLBCL, NOS
Answer:
B. Acute EBV infection (infectious mononucleosis)
Discussion:
After discussion with the clinician, the patient was tested for EBV-specific antibodies:
VCA1 IgM: HIGH
VCA1 IgG: HIGH
EBNA2 IgG: Normal
EA3 IgG: HIGH
1viral capsid antigen; 2nuclear antigen; 3early antigen
The serology, together with other clinical findings, confirmed lymph node involvement by acute EBV infection (infectious mononucleosis).
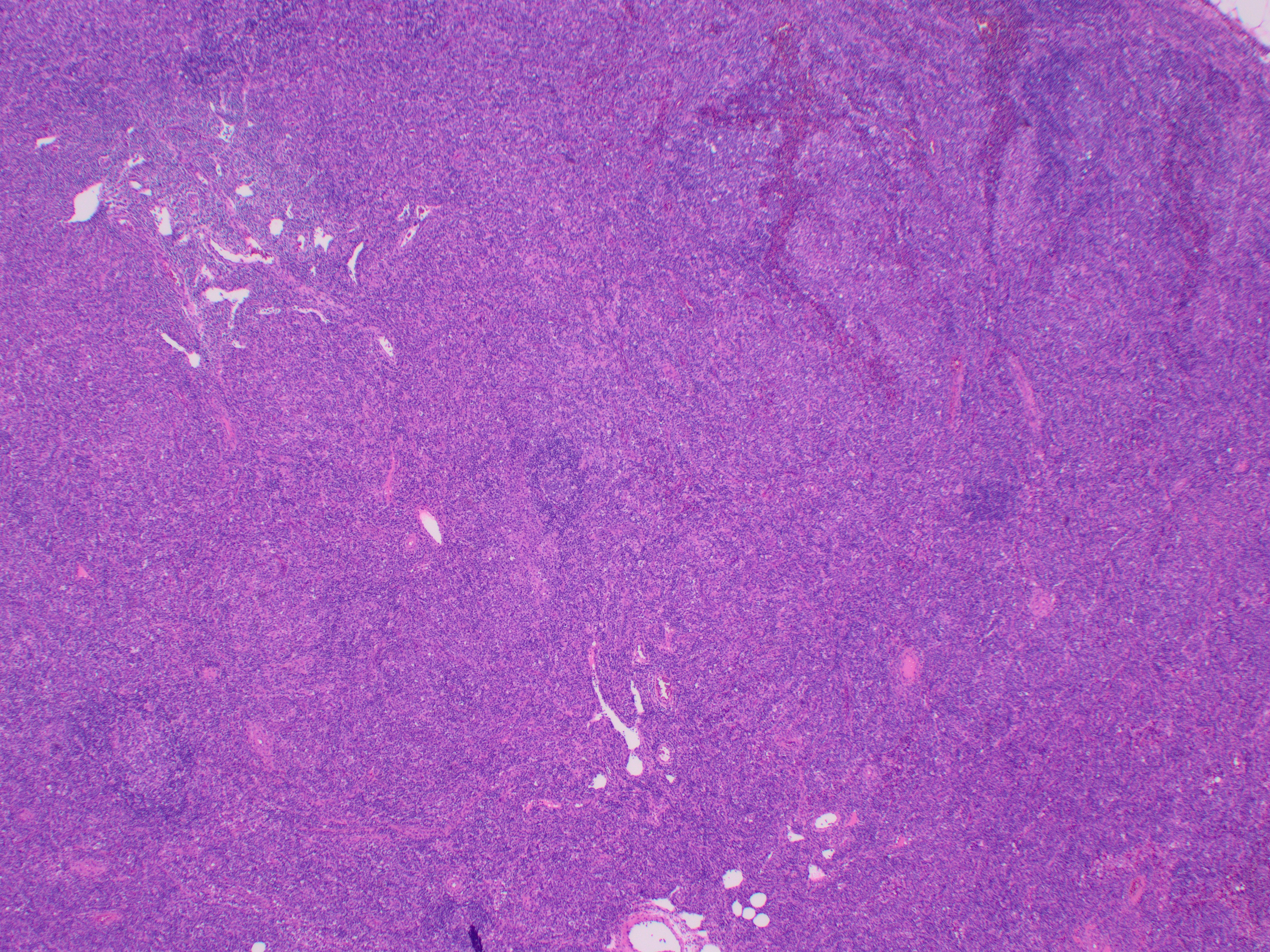
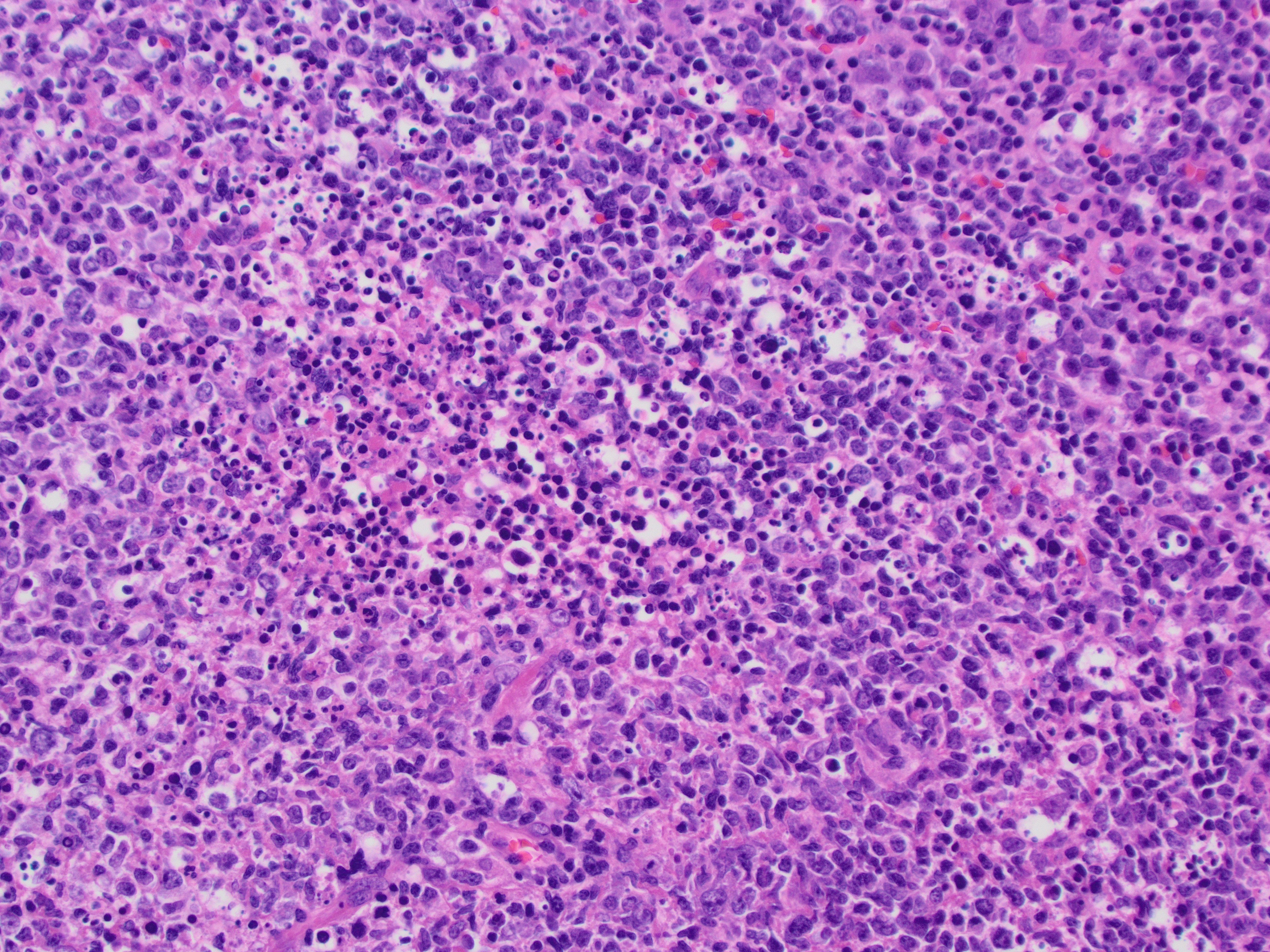
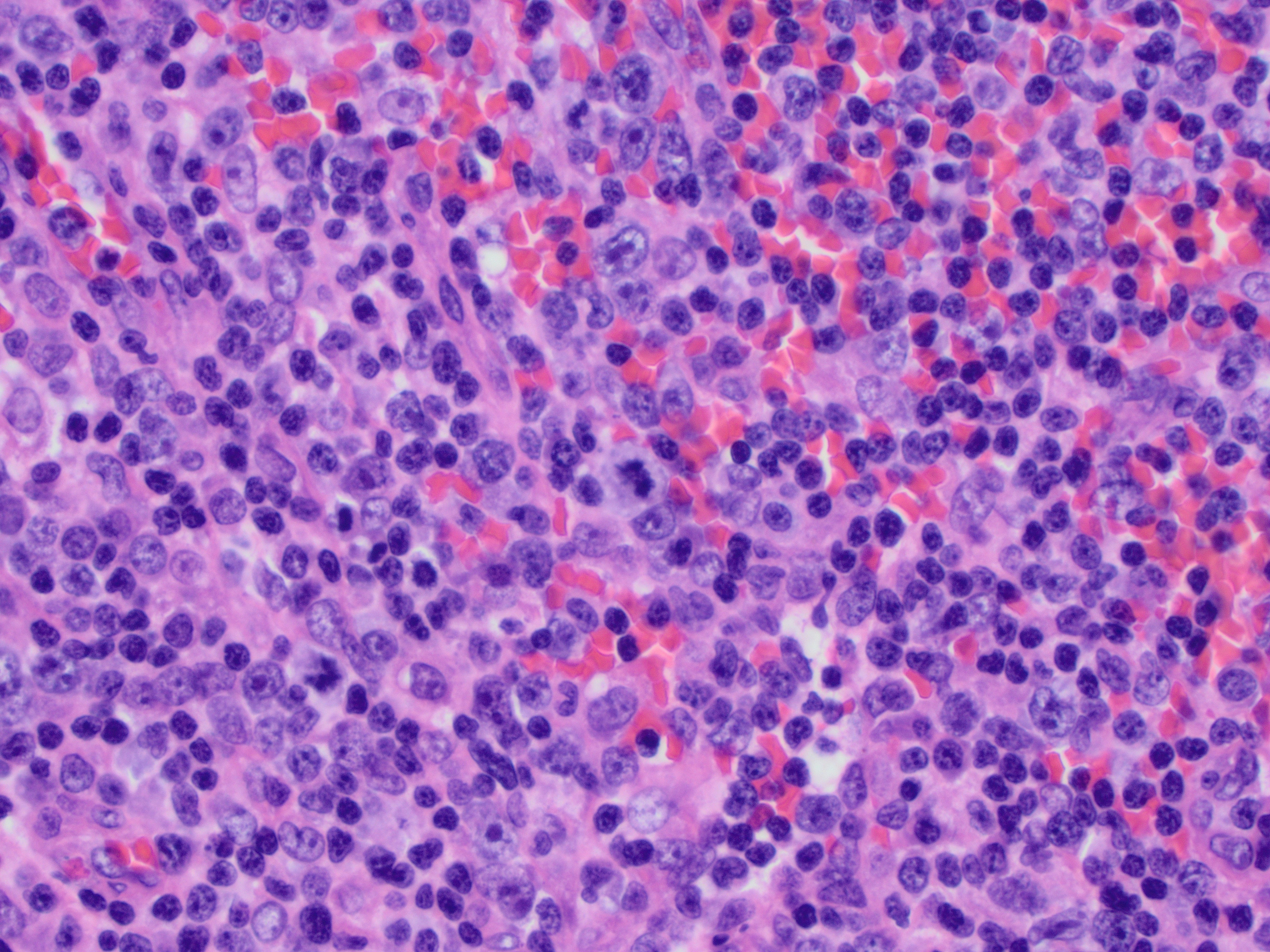
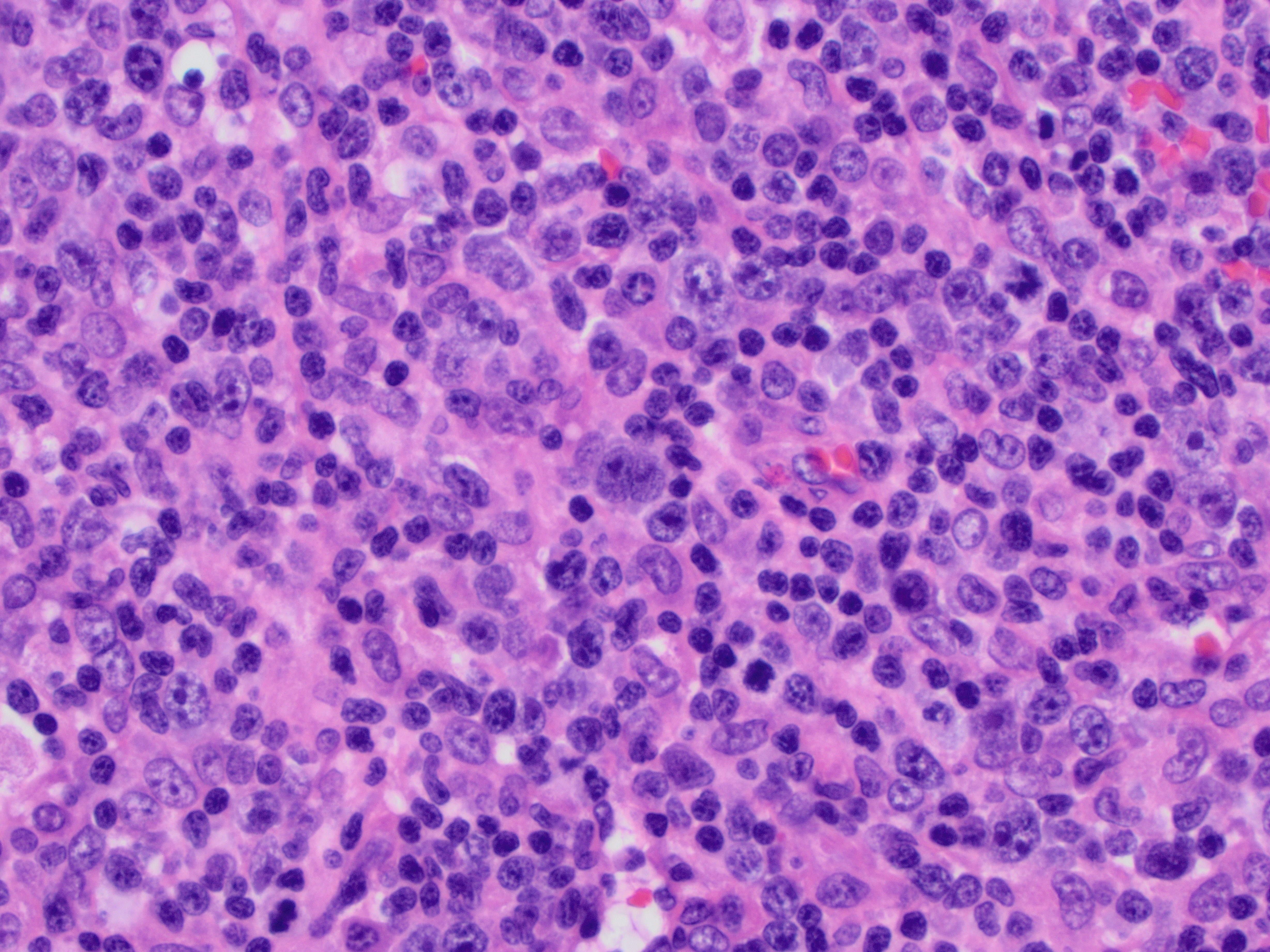
Lymph nodes involved by acute EBV infection characteristically show paracortical expansion by a polymorphous infiltrate of lymphocytes, immunoblasts, plasma cells, and histiocytes. A diagnostic challenge, the immunoblastic proliferation and distorted architecture may be mistaken for a large cell lymphoma. In some cases, extremely large immunoblasts with multilobated/multiple nuclei and prominent nucleoli resemble Reed-Sternberg cells. Key histologic features that support a diagnosis of EBV lymphadenitis include:
- Architectural preservation. While distorted, overall lymph node architecture remains intact.
- Patent sinuses.
- Spectrum of sizes of atypical lymphocytes.
- Immunoblasts include both B- and T-cells on IHC.
- Ki-67 increased. Ki-67 is helpful when distinguishing from Hodgkin lymphoma, which should have a low Ki-67 index in the background normal lymphocytes.