Case History
Placenta from a 38-year-old female delivered at 37 weeks. Maternal history of gestational hypertension and preeclampsia. Gross exam revealed a dark subchorionic placental nodule.
The findings are characteristic of:
- Focal chorangiosis
- Chorangioma
- Chorangiocarcinoma
- Villous infarct
- Laminated intervillous hematoma
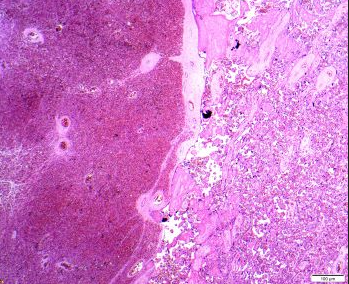


Answer: B. Chorangioma
Chorangiomas are the most common placental tumors (0.5-1%). These benign lesions are reactive in nature and associated with preeclampsia, multiple gestation, and high altitude. Placental hypoxia is the predisposing factor with activation of angiogenesis and excessive capillary proliferation. As a consequence, on gross inspection, chorangiomas tend to be found under the chorionic plate or at the placental margin, sites of reduced oxygenation. In general, they are small (<1 cm) and asymptomatic. Large chorangiomas can cause arteriovenous shunt and platelet trapping with fetal thrombocytopenia, hemorrhage, and disseminated intravascular coagulation.
Histologically, the vascular proliferation expands mature stem villi and is composed of capillary-sized vessels in a collagenous stroma. The small capillaries may be surrounded by pericytes. Mitosis and atypia may be seen, but do not indicate malignant potential. The throphoblast surrounding chorangiomas can show hyperplastic changes, but no atypia or necrosis.
Chorangiomas and infantile hemangiomas appear to be related, often occur concurrently, and share identical tissue-specific markers. It has been proposed that endothelial cells from placental chorangiomas enter the fetal circulation through right-to-left shunts characteristic of the normal fetal circulation, and release growth factors and signaling molecules.
Chrorangiomas are benign hamartomatous mesenchymal lesions that show normal karyotype. Clonality has not been demonstrated in these lesions. Some chorangiomas can undergo infarction and spontaneous regression.
Chorangiosis refers to a diffuse villous hypercapillarization that occurs in mature placentas. Villi are hypervascular and the capillaries are not surrounded by pericytes. There are histologic criteria for the diagnosis known as “the rule of 10”: ≥ 10 medium-powered fields of placental parenchyma with ≥ 10 terminal villi, each containing ≥ capillaries, in at least 3 areas. Chorangiosis is seen in the setting of maternal diabetes, hypertension, and preeclampsia.
Localized chorangiomatosis has identical histology to chorangiomas, but conforms to the outline of the involved stem villi without nodule formation. It is usually not identified by gross inspection. Capillary proliferation is seen inside the involved villi surrounded by pericytes and reticulin fibers.
Chorangiocarcinoma is an extremely rare lesion of intraplacental choriocarcinoma with hypervascular villous stroma. The trophoblast is exuberant with extensive necrosis.
In villous infarcts, the loss of intervillous space with agglutination of dead villi, and associated hemorrhage can rarely be confused histologically with chorangioma. However, chorangiomas may have the appearance of infarcts on gross exam. Attention to detail, such as color and circumscription, may help.
Laminated intervillous hematoma is composed histologically of layers of fibrin and red blood cells without vascular proliferation.
References:
Heerema-Mckenney A., Popek E.J., and De Paepe M.E. 2019. Diagnostic Pathology Placenta. Second Ed. Philadelphia(PA). Elsevier.
Amer HZM, Heller DS. Chorangioma and related vascular lesions of the placenta – A Review. Fetal Pediatr Pathol.2010;29:199-206.
North PE, Waner M, Mizeracki, et al. A unique microvascular phenotype shared by juvenile hemangiomas and human placenta. Arch Dermatol. 2001;137(5):559-570.
Ogino S, Redline RW. Villous capillary lesions of the placenta: distinctions between chorangioma, chorangiomatosis, and chorangiosis. Hum Pathol. 2000 Aug;31(8):945-54.
