Commencement was virtual for fall 2020, but Chris Sims, DNP, and Cecelia Sims, DNP, grabbed a chance to pose in their regalia above University Boulevard. The married couple have earned multiple degrees during their time at UAB and credit the university's educational assistance benefit for playing a major role. Image courtesy Chris SimsEducation represents a path forward for all UAB students, and the university’s employees are no exception. Each year, some 2,700 UAB employees and their dependents use the university’s educational assistance benefit. For many employees, pursuing additional training in the university’s world-renowned programs is a crucial part of their career planning. It can also prepare them to better help others.
Commencement was virtual for fall 2020, but Chris Sims, DNP, and Cecelia Sims, DNP, grabbed a chance to pose in their regalia above University Boulevard. The married couple have earned multiple degrees during their time at UAB and credit the university's educational assistance benefit for playing a major role. Image courtesy Chris SimsEducation represents a path forward for all UAB students, and the university’s employees are no exception. Each year, some 2,700 UAB employees and their dependents use the university’s educational assistance benefit. For many employees, pursuing additional training in the university’s world-renowned programs is a crucial part of their career planning. It can also prepare them to better help others.
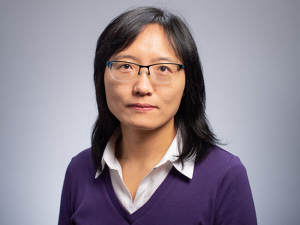
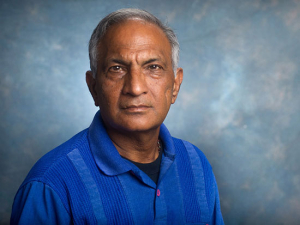
On Dec. 11, nearly 900 master’s and doctoral students — including dozens of UAB employees — capped at least one portion of their educational journeys in a virtual graduate commencement ceremony. Cecelia and Chris Sims, married nurses who work in infection control and anesthesia, respectively, at UAB Hospital, earned matching Doctor of Nursing Practice degrees. Sharon Samuel, a researcher in the Department of Radiology Small Animal Imaging Facility, earned a master’s degree in health physics. And transplant nurse Katie Stegner earned a master’s degree in Public Health with a concentration in health care organization and policy. How did they manage to finish off their studies in the midst of a global pandemic? These new graduates answer that question and more below.
Why did you decide to pursue a new degree?
Chris Sims: "There were multiple reasons. The first was the excellent benefit of employee tuition assistance. My wife and I have been able to use this benefit for multiple degrees. I have used the tuition assistance for my Master’s in Nurse Anesthesia and now the Doctor of Nursing Practice degree. I make it a point in my clinical area to advise new employees to take advantage of this benefit. Few opportunities come along that allow you to obtain a free education. Secondly, I decided to pursue a doctoral degree due to the changes that are occurring in the nursing profession. The American Association of Colleges of Nursing recommends that the entry degree for advanced practice nursing, including nurse anesthesia, is at the doctoral level. Most nurse-anesthesia programs have already transitioned to doctoral degrees. Although nurse anesthetists who completed degrees before this recommendation are not required to obtain a doctoral degree, I decided to pursue a doctoral degree to stay in line with current graduates.”
Cecelia Sims: “I agree with maximizing the tuition assistance benefit as a UAB employee. The DNP is the first degree we have obtained without accumulating any debt. I also watched some of my peers that I attended undergraduate and graduate school with move towards advancing their nursing degrees. Their actions motivated me to apply and pursue a DNP degree.”
Related storiesFor these employees seeking degrees, 2020 brings stress — and success Considering taking a class — or getting a new degree? Read these 10 FAQs about educational assistance at UAB. |
Katie Stegner: “I chose to get my MPH because I knew that what I would learn would help me and help my patients.” [Stegner is an assistant nurse manager and transplant team leader in Perioperative Services; she works closely with Jayme Locke, M.D., director of the UAB Comprehensive Transplant Institute.] “We are growing our transplant team, which will mean that I have more leadership opportunities and going back to school helps with that. But I also had the chance to learn about Alabama's public health history. I was able to dig deep and learn more and I enjoyed being in school because of that.”
Sharon Samuel: “There were many responsibilities that I had in my position that had expanded over the years, and while I could adapt to these changes, I realized that my knowledge base was limited. I felt that the best way for me to grow in my position and in further employment was to provide myself with more regulatory and scientific knowledge related to my area. After some encouragement from an undergraduate program director, I met with the Health Physics program directors to discuss the possibility of me joining the program part-time. They were very gracious.”
What was it like finishing in the midst of the COVID pandemic?
Samuel: “This was not easy, and I was discouraged many times. I enjoyed being in the classroom and I enjoyed human contact. Going virtual was a big adjustment for me. But I was motivated because I was still learning, and the assigned work was diverse enough to keep me interested. My program was amazing. I kept telling myself to do just a little more and took it one step at a time.”
Stegner: “It was very challenging. It was hard to focus on school and retain the information with all that was going on. The transition to online learning was not a big shift, though, because I have always been in class online due to my work hours — transplant is just too unpredictable. I enjoyed being in school, even if I didn’t enjoy working 14 hours and then going home to write a paper. But the professors were very understanding and, in a few cases when I needed to, I could contact them and they would give me a bit more time.”
Chris Sims: “During March 2020, like everyone else, we watched the world change overnight. [But] for Cecelia and I, the transition of our graduate studies was relatively seamless. The School of Nursing has done an excellent job providing access to the DNP program via online instruction. Prioritizing family obligations, remaining active in our church while working full-time and maintaining school responsibilities was difficult at times. Also, we both have active hobbies, like running, cycling and a new-found love of hiking. Although COVID-19 added a new challenge, Cecelia and I were accustomed to juggling multiple events and managing a work-life balance. Starting the DNP together provided both of us with a built-in motivator and cheerleader. We were typically busy with school assignments or free to do whatever simultaneously, which lessened the strain on our relationship. We both had days where one of us was ready to give up, but we were able to encourage each other during those difficult times. We started together, and we were determined to graduate and walk across the stage together.”
Did you have any particular favorite classes, teachers or experiences with this degree?
Stegner: “I really enjoyed learning about environmental health and the history of Alabama and how issues like water contamination continue to affect our patients. We touched on health disparities in several of my classes, and that is definitely something we see in transplant. I did a lot of my papers and projects on transplantation topics. I would joke that my professors were probably sick of all my transplant stuff; whatever the topic, I would usually be able to tie it back to transplant.”
Samuel: “The teachers in this program are amazing. Each semester they were fair, honest and challenging. They were always supportive and willing to help clarify information from class. My favorite classes were Instrumentation and Radiopharmacy. The next runner-up would be Regulations, Radiation Protection and Radiation Biology.”
Chris Sims: “We both agreed that one of our first classes, Health Policy and Politics, was the most influential. I have a better understanding of how legislation at the state and federal levels can have a constructive or adverse effect on overall patient outcomes. Favorable health care policy and accommodating elected leaders are a vital link in improving health care disparities. Before DNP studies, I rarely noticed legislative activities that may have impacted either my professional practice or the population's health. DNP graduates must position themselves as advocates for improved policy and increase political awareness to ensure that our patients receive optimal health care.”
Cecelia Sims: “One of our biggest supporters as Chris and I matriculated through the DNP program was Dr. Aimee Holland. She always emphasized that teamwork is a vital component in progressing through the program. She always made us aware of our strengths and how to build upon those areas while also realizing that there are professional development areas that may be challenging and how important it is to seek out mentors who could help us overcome those elements. Also our faculty mentors, Dr. Curry Bordelon and Dr. Stephanie Hammond, played critical roles in our success.”
Is there anything else you would like to add?
Samuel: “I received so much support from my department. If they didn’t support me going to school, I wouldn’t have been able to do this. Special thanks to Drs. [Suzanne] Lapi and [Anna] Sorace, who continue to push me forward.”
Cecelia Sims: “My background has always been in pediatric nursing, which led me to become a Certified Pediatric Nurse Practitioner, and I have spent a large portion of my career as a Certified Infection Control Practitioner at UAB. I am the Lead Infection Preventionist over the Women and Infant Services and Rehabilitation Services. My role involves collaborating with different departments within the UAB Health System, formulating strategies to keep our patients safe and decreasing the risk of a hospital-acquired infection. The knowledge and skills I obtained in the DNP program will allow me to develop new policies and improve current policies. The ability to communicate efficiently, deploy scholarly knowledge and practice creative thinking have each proven to be useful tools in my current role.”
Chris Sims: “This degree doesn't change my role or how I practice in the clinical setting. However, I have a broader understanding and appreciation for evidence-based practice, organizational leadership, data management and health care policy. The increasing complexity, acuity and need for specialized services to provide optimal patient care requires a multidisciplinary approach. The DNP-prepared practitioner is poised to bridge the gap between the multiple facets of the health care teams that are expected to fulfill the needs of a vast population of patients. The leadership and communications skills developed during my DNP education are essential in leading and consulting interprofessional teams.”
Stegner: “I did my internship for the MPH with Dr. Locke’s lab group. They are implementing a pilot program to help with organ donation, and I was able to help them by making manuals for the coordinators and navigators. I learned more about their Engage program and now I help one of the staff on Saturdays, doing COVID checks and screenings when they have their donor meetings. I was able to get more involved outside of the OR and I enjoyed that. There are lots of exciting things coming up with transplant that Dr. Locke wants to accomplish. When I finished the master’s degree, I told my team, ‘I’m done!’ And one of my team members said, ‘Until she goes back for her doctorate.’ I told them, ‘That will not happen.’ Then again, I did say years ago I wouldn’t get my master’s degree. So you never know.”