Case History
Patient history:
52-year old male received deceased donor kidney transplantation 6 month ago, end stage renal disease secondary to fibrillary glomerulonephritis. Creatinine has been fluctuating between 1.9-2.1 in recent 3 month (the baseline was 1.3 to 1.4). Recent donor specific antibody (DSA) test is negative, and other serologic tests are pending.
Question #1: Based on clinical history, pictures of chemical and IHC stains, which diagnosis is favored:
- A) Acute T cell-mediated rejection.
B) Antibody-mediated rejection.
C) Post-transplant lymphoproliferative disorder.
D) Polyomavirus nephropathy
Question #2:
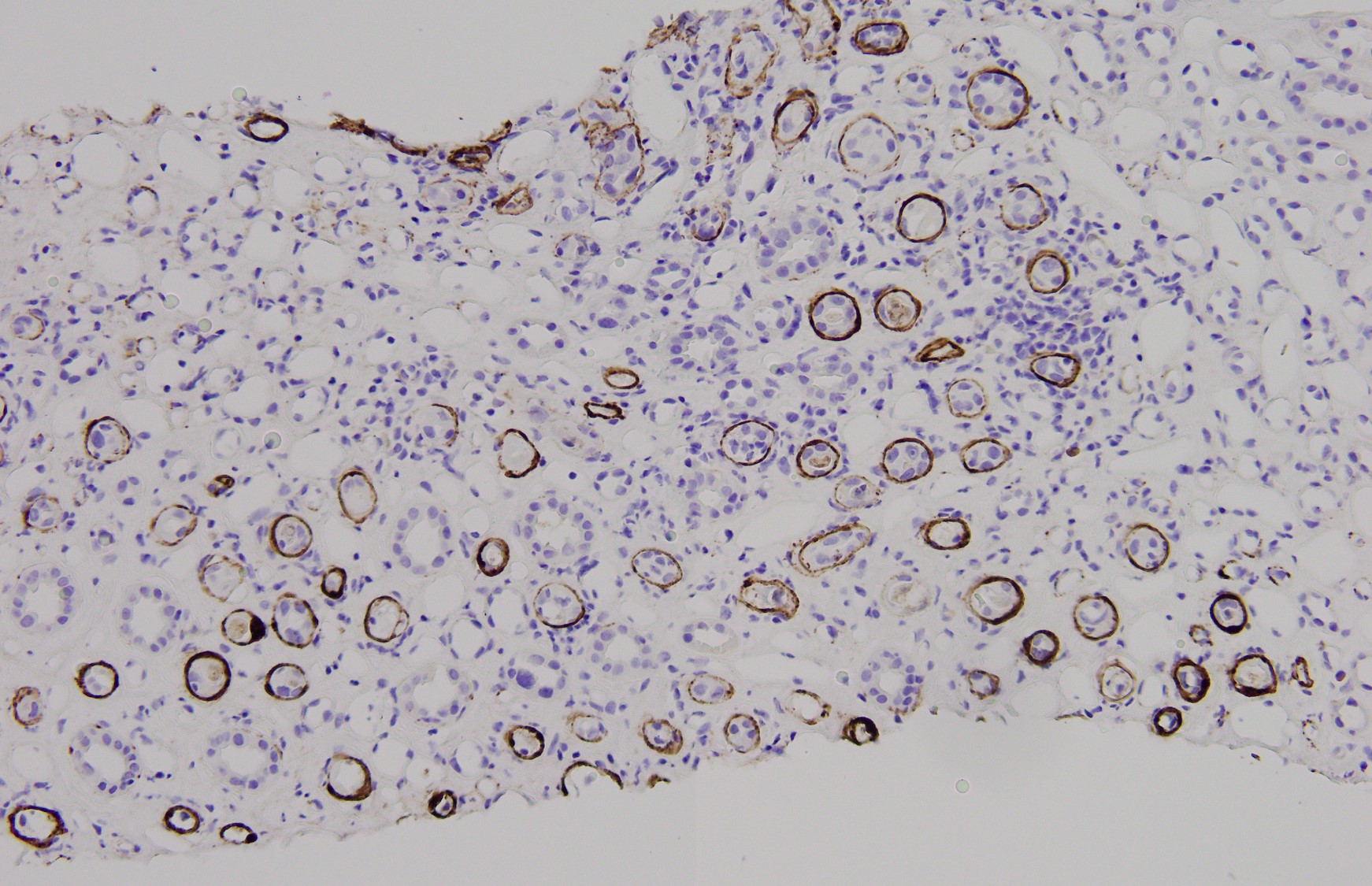
The figure 4 shows a IHC stain for C4d. Based on this picture, a concomitant antibody-mediated rejection will be diagnosed with certainty.
A. Yes
B. No


Answers:
Q1: D. Polyomavirus nephropathy
Q2: B. No
Discussion:
BK polyomavirus is a small DNA virus that establishes lifelong infection in the renal tubular and uroepithelial cells of most of the world's population. For the majority of healthy people, infection is quiescent and benign. However, in immunocompromised patients, especially among renal transplant recipients, viral reactivation is common. Reactivation is frequently subclinical, or without systems at all, so screening for reactivation is recommended for all recipients after renal transplantation. The viral replication usually occurs in the first year following transplant, especially within the first 6 months. The stereotypical pattern of clinical manifestations of this infection is viruria, followed by viremia, and finally with virus-related nephropathy. For those with significant clinical symtoms of plasm PCR/tissue biopsy confirmed, reduction of immunosuppression is the cornerstone of management. There is no specific antiviral or immunomodulatory therapy sufficiently effective for routine use.
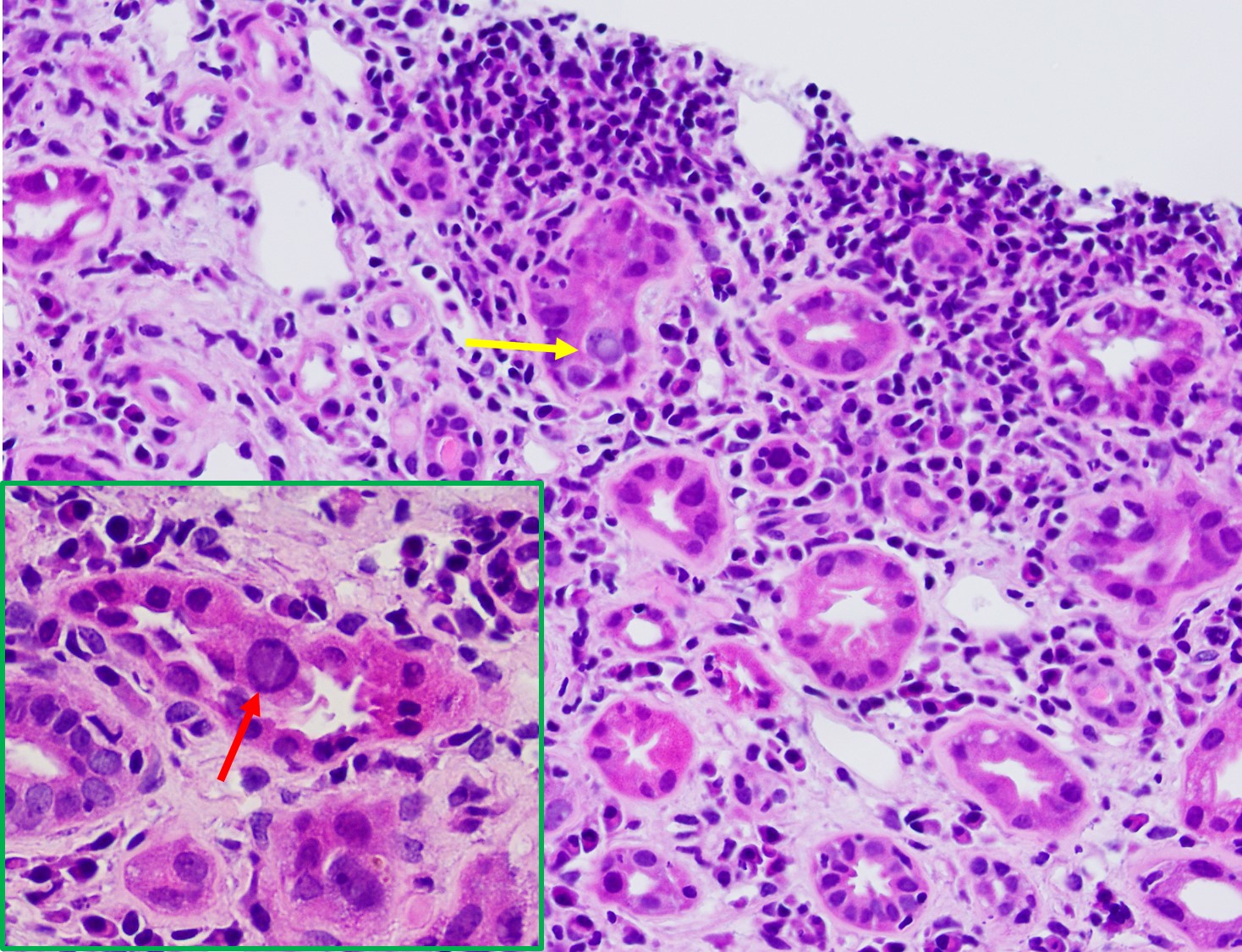
It is not always easy of straightforward to distinguish BK nephropathy from acute rejection, and very difficult to diagnose a coexisting lesion including both of them. T cell-mediated rejection shares similar histopathologic features with BK nephropathy, such as focal and brisk interstitial inflammation and tubulitis (shown in Fig. 1). However, typical viral cytopathic changes are more common in BK nephropathy, such as nuclear enlargement and intranuclear infusion (Fig. 2, yellow arrow) and features resenbling so called "decoy cells" in urine cytology (Fig. 2, red arrow). SV-40 large T antigen staining with IHC confirms a diagnosis of polyomavirus infection (shown in Fig. 3), but can't differentiate BK from JC virus. Interestingly, some patients with BK nephropathy shows C4d deposits in the tubular basement membrane (Fig. 4), but not the typical pattern of peritubular linear C4d stain for antibody-mediate rejection.
Case contributed by: Bo Chen, MD, PhD, Instructor & Fellow, Surgical Pathology