Case History
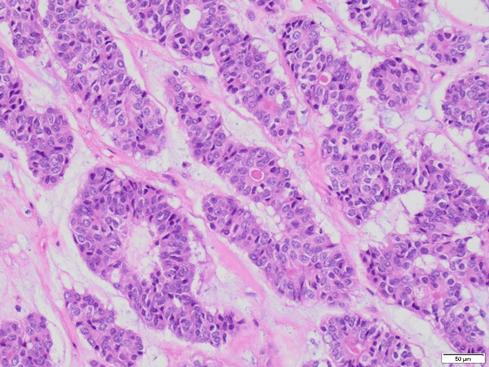
A 60-year-old woman presents with urinary symptoms, abdominal distension and bloating. A CT scan shows a large pelvic mass. A bilateral salpingo-oophorectomy with omentectomy is performed and reveals a 27.5 x 22.5 x 17.9 cm white, firm, and solid mass in the left ovary. Immunohistochemical staining shows positivity with pan-cytokeratin, CAM5.2, ER, PR, WT1, and PAX8 (patchy). Beta-catenin shows nuclear patchy staining. Calretinin, inhibin, and SF-1 are negative in neoplastic cells. The neoplastic cells are negative for GATA3, TTF-1, CDX2, INSM1, chromogranin, and synaptophysin.
What is the most likely diagnosis?
A. Wolffian tumor of the ovary
B. Mesonephric-like carcinoma
C. Endometrioid carcinoma with sex cord-like pattern
D. Sertoli/Sertoli-Leydig cell tumor
E. Metastatic carcinoma
Correct answer: C. Endometrioid carcinoma with sex cord-like pattern
Discussion:
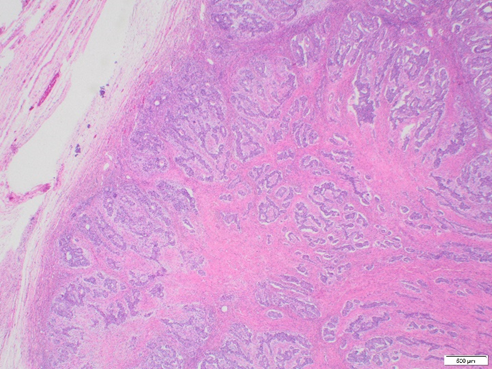
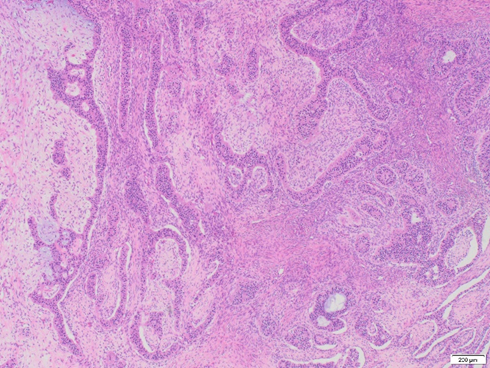
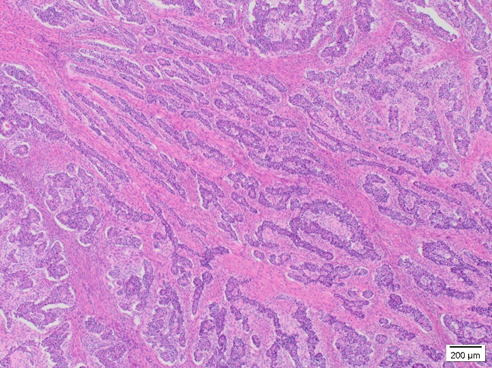
Endometrioid carcinomas are morphologically heterogeneous, with a spectrum of appearances similar to those seen in endometrioid carcinomas of the uterus, potentially constituting a diagnostic pitfall (Malpica, 2016). On rare occasions, endometrioid carcinoma mimics sex cord-stromal tumors, a common scenario encountered in the ovary. These tumors can form solid or hollow tubules, nests, and elongated cords, such as in our case.
The distinction between endometrioid carcinoma with a sex cord pattern and a true sex cord-stromal tumor is based on recognizing this unconventional architecture and confirmation with immunohistochemical stains. The tumor is frequently positive for EMA and cytokeratins and negative for sex cord markers. Although PAX8 may be often negative, ER, PR, beta-catenin, and CD10 has been expressed most studies (Travaglino et al., 2024). Despite its unusual morphology, endometrioid carcinoma with a sex cord pattern typically behaves as a low-grade tumor and shows an excellent prognosis when confined to the ovary (Young et al., 1982).
Wolffian tumor of the ovary (formerly known as female adnexal tumor of probable adnexal origin, FATWO) is a rare entity that may show overlapping features with endometrioid carcinoma with sex cord pattern. Morphologically, paratubal location (where mesonephric remnants may be present), multilobated architecture, bland nuclear features, and low mitotic index are features of FATWO. By immunohistochemistry, these tumors are also variable. They can be positive for pan-cytokeratin and vimentin. EMA, ER, and PR are negative or only focally positive, while AR is diffusely positive. Calretinin, inhibin, and WT-1 are positive, but GATA3, PAX8 and SF1 are usually negative (Goyal et al., 2016).
In brief, features that may be helpful in diagnosing mesonephric-like carcinoma include atypia, a high mitotic count, GATA3 and TTF1 positivity, and molecular studies showing KRAS/NRAS mutation.
Lastly, a metastatic carcinoma should always be considered when an ovarian carcinoma with unusual morphology is encountered. Small ovarian size, bilaterality, multinodular configuration, surface involvement, and destructive stromal invasion are helpful morphologic criteria favoring metastasis. An appropriate clinical history and immunohistochemical markers can help in the differential.
Resources:
Goyal, A., Masand, R. P., & Roma, A. A. (2016). Value of PAX-8 and SF-1 Immunohistochemistry in the Distinction Between Female Adnexal Tumor of Probable Wolffian Origin and its Mimics. Int J Gynecol Pathol, 35(2), 167-175. https://doi.org/10.1097/pgp.0000000000000222
Malpica, A. (2016). How to approach the many faces of endometrioid carcinoma. Mod Pathol, 29 Suppl 1, S29-44. https://doi.org/10.1038/modpathol.2015.142
Travaglino, A., Arciuolo, D., Santoro, A., Fulgione, C., Piermattei, A., Martinelli, M., Onori, M. E., Minucci, A., Raffone, A., Inzani, F., & Zannoni, G. F. (2024). Ovarian endometrioid carcinoma with a sex cord-like pattern: a morphological, immunohistochemical, and molecular analysis. Virchows Arch. https://doi.org/10.1007/s00428-024-03743-6
Young, R. H., Prat, J., & Scully, R. E. (1982). Ovarian endometrioid carcinomas resembling sex cord-stromal tumors. A clinicopathological analysis of 13 cases. Am J Surg Pathol, 6(6), 513-522. https://doi.org/10.1097/00000478-198209000-00003
Case contributed by: Valeria Dal Zotto, M.D., Assistant Professor, Anatomic Pathology, UAB Pathology