Case History
A 73-year-old male with a history of relapsed/refractory NK T-cell lymphoma, s/p chemo and immune checkpoint inhibitors therapy. The patient now presents with new onset nephrotic syndrome and acute kidney injury.
What is the most appropriate diagnosis?
A. Granular casts associated with acute tubular necrosis
B. Acute interstitial nephritis
C. Light chain cast nephropathy
D. Myoglobin casts
Correct answer: C. Light chain cast nephropathy
Discussion:
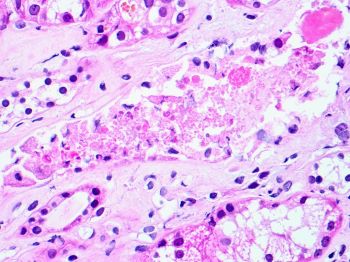
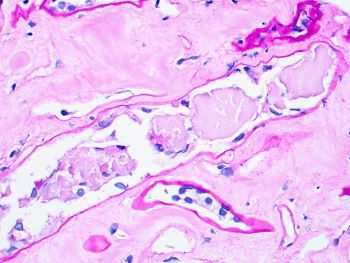
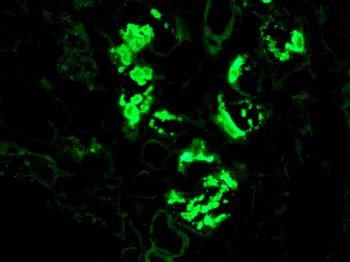
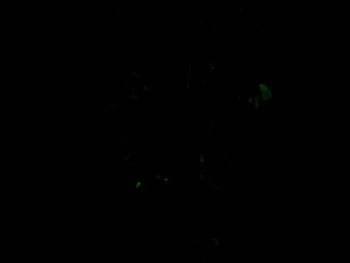
Granular casts (Fig a) are commonly seen in association with acute tubular necrosis because of degenerating sloughed off tubular epithelial cells and can be identified on routine urinalysis. However, these are strong PASH positive. Myoglobin casts are usually pale PASH staining; however, they do not have fractured, angulated appearance (Fig b) or light chain restricted staining by immunofluorescence (Fig c and d). Therefore, the morphologic features by light microscopy and immunofluorescence are supportive of light chain cast nephropathy (LCCN). Although light chain casts typically show metachromatic (two-tone) or pale PASH staining and syncytial giant cell reaction, early on these casts may have granular appearance and are surrounded by PMNs, as shown in Fig a (arrows).
This is an unusual case as LCCN is the most common renal manifestation of neoplasms associated with abnormal production of light chains i.e., plasma cell dyscrasias and lymphomas with plasma cell differentiation e.g., lymphoplasmacytic lymphoma. However, this patient had a history of NK T-cell lymphoma. Although bidirectional risks of developing B- and T-cell lymphomas (BCLs and TCLs) are less well understood, recent studies have shown nearly fivefold increased bidirectional risk between BCL and TCL overall. The risk is strongly associated with the specific lymphoma subtype, with particularly high reciprocal risks for peripheral T cells lymphoma and angioimmunoblastic lymphoma among T-cell lymphomas. Also there is increased risk within 1 year after first lymphoma, suggestive of a surveillance effect or subsequently diagnosed composite lymphoma. These observations raises the possibility of shared predisposition and/or exposure(s) leading to the increased reciprocal risk of specific lymphoma subtypes.
Reference:
Dai Chihara, Graça M. Dores, Christopher R. Flowers and Lindsay M. Morton. The bidirectional increased risk of B-cell lymphoma and T-cell lymphoma. Blood (2021) 138 (9): 785–789.
Case contributed by: Huma Fatima, M.D., Associate Professor, Renal Section Head, Anatomic Pathology, UAB Pathology