Imagine being discharged from the hospital knowing you suffer from heart failure, and you have no access to continuing outpatient care. What do you do when you’re in trouble—go to the emergency room, get readmitted, or worse, do nothing? It’s a recipe for a vicious cycle that could have disastrous outcomes.
UAB patients will soon have support to prevent that from happening. Born of the UAB Nursing academic practice partnership between the School and UAB Hospital, a new nurse-managed, population-based transitional care clinic for heart failure patients recently discharged from UAB Hospital is opening in September 2014, supported by a $1.5 million Nurse Education Practice Quality Retention (NEPQR) grant from the Health Resources and Services Administration (HRSA).
 An interprofessional team of nursing, medicine, social work, health services administration and health information technology professionals, comprises this innovative, replicable collaborative practice model clinic and targets the underinsured and medically underserved. The three-day-per-week clinic and its around-the-clock transitional care support fill a much-needed gap.
An interprofessional team of nursing, medicine, social work, health services administration and health information technology professionals, comprises this innovative, replicable collaborative practice model clinic and targets the underinsured and medically underserved. The three-day-per-week clinic and its around-the-clock transitional care support fill a much-needed gap.
“Recent closure of the regional indigent-care hospital, Cooper Green Mercy Hospital, has created a critical access issue for this vulnerable population,” said the project’s director, Maria Shirey, PhD, RN, FAAN, Assistant Dean for Clinical and Global Partnerships. “The School already has experience leading the successful nurse-managed PATH clinic at M-POWER Ministries, geared to a population with diabetes. This new clinic expands our reach, serving as a ‘hub’ for transitional care coordination services for a high-risk population of heart failure patients across the hospital, clinic, home and community.”
Over the past several years, UAB has been monitoring clinical outcomes in heart failure patients, said Connie White-Williams, PhD, RN, FAAN, Director of the Center for Nursing Excellence at UAB Hospital and Shirey’s partner in the project. Inconsistent length of hospital stays have been observed, along with higher-than-desired readmission rates. Traditional quality efforts, she said, have only modestly improved the rates and further development of new, more effective strategies is needed.
“We believe this model with its around- the-clock transitional care coordination across the hospital, clinic and home will be effective in keeping patients at home and as healthy as possible,” Shirey added. “And what we learn from this initiative can ultimately change the existing model of care to benefit all heart failure patients.”
Transitional care coordination begins while patients are still in the hospital, Shirey said. A clinical nurse leader will serve as a case manager to coordinate care across the health care continuum and be on call for issues that may arise after clinic hours. Nurse practitioners will see patients during clinic hours and make daily inpatient rounds on eligible heart failure patients at UAB Hospital.
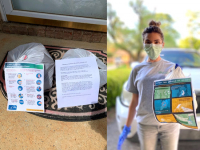
Team members also will evaluate patients for palliative care eligibility, and contact them within 48 hours of hospital discharges to ascertain their well-being and confirm scheduled follow-up clinic visits. “A nurse practitioner then will make an initial home visit to assess the patient’s status and social support, as well as other issues that could impact his or her health, including not having air conditioning, or even something as simple as not having a scale on which to weigh,” she said.
Shirey added the population-based transitional care team will use the hospital’s new EMMI Solutions technology, an automated voice-response technology, to set up electronic patient phone call reminders to trigger self-reported weigh-ins and provide reminders about appointments and care recommendations. EMMI is already being used at UAB Hospital for other patient populations.
A unique aspect of the clinic, Shirey said, is the incorporation of palliative care services. UAB School of Nursing Marie O’Koren Endowed Chair Marie Bakitas, DNSc, NP-C, FAAN, has an internationally recognized, NIH-funded program of research focused on delivering targeted palliative care interventions customized for heart failure patients and their caregivers. Bakitas will help the team to integrate palliative care principles into all aspects of care to help improve quality of life for both the patients and their families.
As part of a world-class academic medical center, there also is an educational component to the clinic. Graduate nursing and health systems administration students from the School of Nursing and School of Health Professions will be involved during the project start-up phase—conducting needs assessments, performing information flow and workflow analyses, ensuring the operability of electronic medical records, and developing and implementing a plan for smooth clinic operations. Eventually, a variety of students will be incorporated as members of the health care team. This includes bachelor’s through doctoral nursing students, bachelor’s-level social work students, and medical residents and fellows in cardiology. They will participate in morning team huddles and afternoon post-conferences, and will provide input on team functioning at the end of each clinic day.
Team members for the clinic also include UAB School of Nursing Assistant Professor Shea Polancich, PhD, an expert on quality and safety, and UAB cardiologist Vera Bittner, MD, the clinic’s collaborating physician.