The same protein tells beta cells in the pancreas to stop making insulin and then to self-destruct as diabetes worsens, according to a UAB study published online Aug. 23, 2013 in the journal Nature Medicine.
The same protein tells beta cells in the pancreas to stop making insulin and then to self-destruct as diabetes worsens, according to a UAB study published online Aug. 23, 2013 in the journal Nature Medicine.
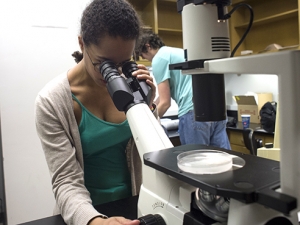
Specifically, the research revealed that a protein called TXNIP controls the ability of beta cells to make insulin, the hormone that regulates blood-sugar levels.
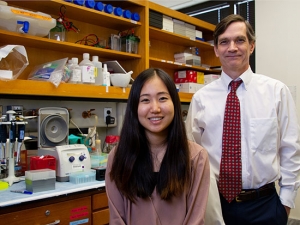
“We spent years confirming that TXNIP drives beta-cell death in both Type 1 and Type 2 diabetes,” said Anath Shalev, M.D., director of the UAB Comprehensive Diabetes Center and senior author of the paper. “We were astounded to find that its action also contributes to a second major diabetic mechanism — the decrease seen in insulin production by beta cells — by a mechanism never before seen.”
During their research, Shalev and colleagues discovered that high TXNIP triggers beta cells to make a specific snippet of genetic material called microRNA-204.
Genetic instructions are encoded in DNA chains and converted into ribonucleic acids (RNA) that direct the building of the proteins that comprise bodily structures and signals. A large portion of human genetic material, however, does not encode proteins and once was considered “junk DNA.” RNA snippets called microRNAs are built based on this junk DNA, but instead of converting its messages into proteins, they silence targeted genes. This provides yet another level of regulation and a tool to turn genes on or off.
The study found that microRNA-204, in response to the TXNIP signal, interferes with MAFA, a transcription factor known to turn on the insulin gene. This is not the first instance of a microRNA influencing a transcription factor, but is a first for a factor critical to the expression of the human insulin gene. Taken together, the evidence argues for the existence of a previously unknown TXNIP/miR-204/MAFA pathway that dials down insulin production and drives diabetic disease.
Read more about the study and its findings.