 Each year, more than 250,000 Americans will injure an ACL. But the principles of ACL care have shifted in recent years, including immediate movement after surgery but longer waits before return to play.
Each year, more than 250,000 Americans will injure an ACL. But the principles of ACL care have shifted in recent years, including immediate movement after surgery but longer waits before return to play.
Here is a good way to tear your ACL: In a pickup basketball game, jump for a rebound and then land awkwardly on someone else’s foot. Or you might plant your leg for a quick cut playing soccer. You feel a pop, your knee seems to give out and suddenly you are on the ground and, often, in intense pain. Then the swelling starts.
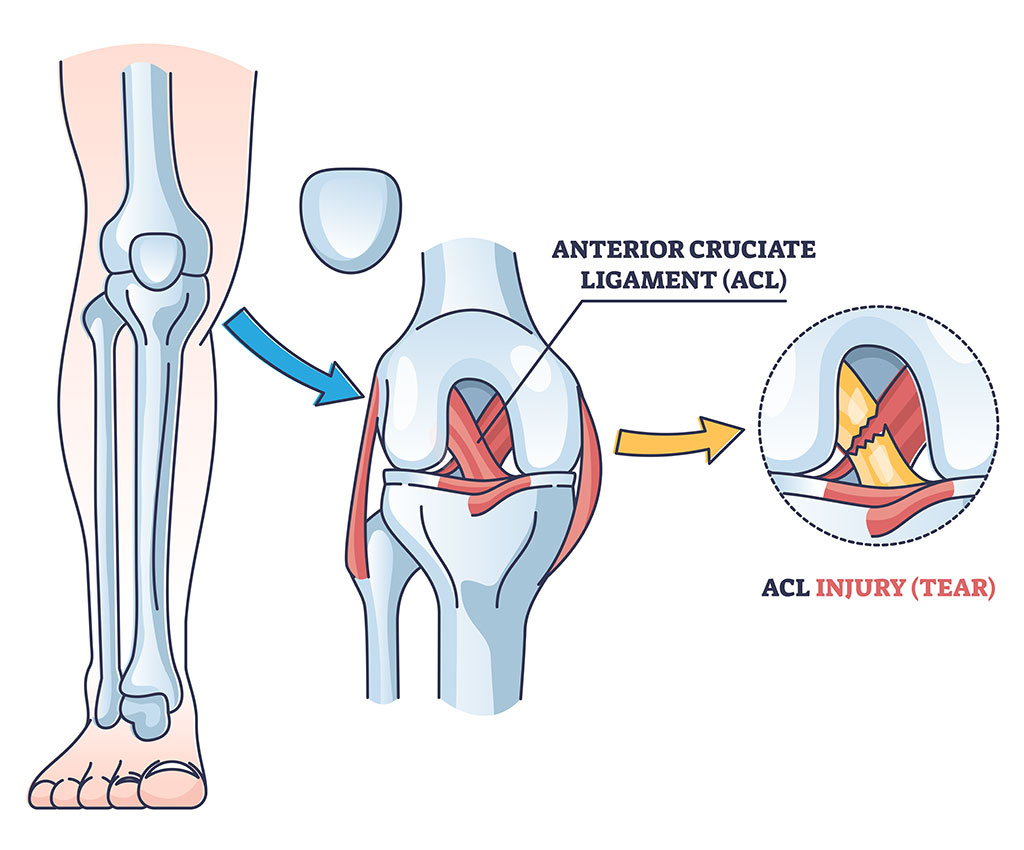
The ACL, or anterior cruciate ligament, connects the big thigh bone, the femur, to the tibia, also known as the shinbone. It is made tough, able to withstand up to 500 pounds of pressure; but intense or awkward jumping or cutting movements can burst through that ceiling and tear the ACL.
So far, so common: Each year, more than 250,000 Americans will injure an ACL. Some of them will just need rest, but other injuries are serious enough to require surgical reconstruction and months of rehabilitation. And this is where the field is experiencing constant change.
Here, two UAB experts — physical therapist Justin Kirk, DPT, and orthopedic surgeon Amit Momaya, M.D. — explain how ACL care has shifted in recent years and the new standards being set at elite medical centers such as UAB.
Bad waiting and good waiting
 Justin Kirk, Ph.D. Image courtesy TherapySouthIn a recent episode of the UAB MedCast podcast, UAB physical therapist Justin Kirk, DPT, explained that, roughly half of the time, ACL tears are misdiagnosed as knee sprains. “It’s not until a little bit later, when things are not clearing up, the swelling is not going down, the knee is still buckling” that patients get an MRI and the ACL tear is correctly diagnosed, Kirk said.
Justin Kirk, Ph.D. Image courtesy TherapySouthIn a recent episode of the UAB MedCast podcast, UAB physical therapist Justin Kirk, DPT, explained that, roughly half of the time, ACL tears are misdiagnosed as knee sprains. “It’s not until a little bit later, when things are not clearing up, the swelling is not going down, the knee is still buckling” that patients get an MRI and the ACL tear is correctly diagnosed, Kirk said.
What then? Direct to surgery? “The best evidence now is suggesting that, unless you have a very tight timeline, to go ahead and not go directly into surgery on day one after the injury,” Kirk said. “Let some of that inflammation cool off and then get a ‘quiet knee’ and then perform the surgery … after, hopefully, you have gained a little bit more of your quad strength back.”
Get moving quickly after surgery
“Stereotypically, in years past, they would cast you after an ACL [surgery] or put you on bedrest and tell you to not move the knee at all,” Kirk said. “Now, most of the time, we [physical therapists] are seeing these patients day one post-op and immediately getting them to bend their knee, much to their surprise.”
But wait before return to play
 Amit Momaya, M.D. (center, holding football) and members of the Sports Medicine staff of the Blazers football team in 2020. Momaya works closely with professional athletes playing for Birmingham's Legion FC soccer team, the Birmingham Bulls hockey team and the USFL. Previously, return-to-play guidelines after ACL surgery suggested waiting around six months, Kirk says. But in the past five years, that recommendation has moved out “around nine months,” he said. “That’s just what it takes to regain that strength and focus on the ankles, the hip rotators, the quads and just get everything up to speed.”
Amit Momaya, M.D. (center, holding football) and members of the Sports Medicine staff of the Blazers football team in 2020. Momaya works closely with professional athletes playing for Birmingham's Legion FC soccer team, the Birmingham Bulls hockey team and the USFL. Previously, return-to-play guidelines after ACL surgery suggested waiting around six months, Kirk says. But in the past five years, that recommendation has moved out “around nine months,” he said. “That’s just what it takes to regain that strength and focus on the ankles, the hip rotators, the quads and just get everything up to speed.”
Momaya, who is section chief of Sports Medicine in the UAB Department of Orthopaedic Surgery, works closely with professional athletes playing for Birmingham’s Legion FC soccer team, the Birmingham Bulls hockey team and the USFL football league, which spent its entire inaugural season at Protective Stadium in Birmingham. Momaya said that he recommends “return to play at around nine to 12 months or later, even for elite athletes.”
Changing timeframe, changing graft choices
Without the rush to get an athlete ready to return to play in six months, there has been a shift in the grafts surgeons use. “They used to use the patellar ligament graft for the bone-tendon-bone anchor, because it could heal and be ready by six months,” Kirk said. “But now … the emerging graft is the quad tendon graft. Dr. Momaya has been doing these, and we have been seeing a lot of his patients who have had that [done], and it seems to be getting a really nice, stable knee without that residual anterior knee pain that a lot of people talk about as one of the most prominent [aftereffects] of an ACL reconstruction.”
Momaya regularly works with both elite and recreational athletes after ACL injuries. “I use both patellar tendon grafts and quad tendon grafts, but I am one of the most frequent users of the quad tendon in the Southeast,” he said. “Some of the advantages of the quad tendon include increased collagen and thickness, less pain at the harvest site, and the ability to pick the length of the graft.”
Several factors go into the graft choice, Momaya says, but some that weight the argument in favor of a quad tendon graft include if a patient has an abnormally long patellar tendon, the patient’s history of patellar tendinitis and whether or not the patient has a small patella bone (in which case, using the quad tendon could avoid a potential patella fracture).
Reducing risk of re-tears with LET
In addition to ACL reconstruction, Momaya often performs a lateral extra-articular tenodesis, or LET, procedure for patients who are good candidates. The LET provides greater stability to the knee from rotational forces and takes stress off of the ACL graft, he says. “My team and I started performing the procedure for athletes about four years ago and have seen terrific results,” Momaya explained. “The majority of sports medicine surgeons in Alabama do not routinely use the LET procedure,” he added.
In addition to serious athletes, any patient may potentially “benefit from LET to reduce re-rupture” if a previous ACL reconstruction has failed, necessitating a revision ACL surgery, Momaya said.
Another recent innovation is use of an internal brace, or “seat belt,” “to help protect the reconstructed ACL,” Momaya said.
Reducing arthritis risk
Risk factors for arthritis post-ACL injury
“Even though we have much to learn about reducing the prevalence of early-onset arthritis after ACL injuries, we know that it’s associated with having a higher BMI [body-mass index], being physically inactive and having a poorly developed muscular system to help absorb the forces we encounter as we go throughout life,” Kirk said. “Weakness in the quadriceps muscle in particular is associated with earlier onset of arthritis. Even though we don’t have a position statement to give clear guidelines, I think it’s generally a good idea to maintain a relatively healthy BMI, stay active and perform regular strength training to help guard against early-onset arthritis.”
One often-cited statistic notes that half of patients who have had ACL repair will have arthritis in that knee within 10 years. “Arthritis rates remain high after ACL injury long-term and may be due to the injury itself as opposed to going through surgery,” Momaya said. “However, in the past decade, we have improved our techniques and are repairing more meniscus tears and placing our ACLs more anatomically, which may change the rate of long-term arthritis.”
What else is new?
“There are plenty of other new developments for ACL treatment,” Momaya noted. These include “drilling more anatomic tunnels, new graft preparation techniques and blood flow restriction after ACL reconstruction to help strength.”
Indeed, blood flow restriction, or BFR, therapy has been a hot topic in gyms, locker rooms and elsewhere, as Momaya has noted on his blog.
To schedule an appointment, call the UAB Sports and Exercise Medicine clinic at (205) 930–8339.
Preventing ACL injuries
 Preventing a non-contact ACL injury — the most common type — may come down to answering one question: “How do you land and absorb force?” Kirk said. “Because that’s all the body is trying to do — it is you versus gravity …. Is gravity dominating you, or can you withstand the forces of gravity and momentum?”
Preventing a non-contact ACL injury — the most common type — may come down to answering one question: “How do you land and absorb force?” Kirk said. “Because that’s all the body is trying to do — it is you versus gravity …. Is gravity dominating you, or can you withstand the forces of gravity and momentum?”
To regain control from gravity, “hamstrings, hip rotators, ankles, glutes, quads, all of these things we really need to be up to full speed to counter the demands of side-to-side rotation and front-to-back motions in sport,” Kirk said.
In fact, “a lot of times, your athletic resilience is directly tied to how good you are on one leg,” Kirk said. “These glaring asymmetries in strength and stability, body control, coordination, how you land on one leg, how you land after you get bumped in the air: They don’t necessarily guarantee an injury, but they do set you up for either risk or success. Some of these injuries are bound to happen no matter what. But if you get really, really good at single-leg movement and exercise and body control, I believe you can prevent some of these avoidable injuries.”
It is critical to work on strength symmetry after an ACL reconstruction as well. Current research “suggests that, if you can get 90 percent or greater on strength symmetry tests, single-leg hop tests, range-of-motion tests for symmetry, single-leg squat tests, your risk for reinjury is significantly less,” Kirk said.