Ben Larimer's passion is the search for new imaging methods to fight cancer and other diseases.If you don’t get excited talking to Ben Larimer, Ph.D., a researcher developing new imaging tests in the UAB Department of Radiology, you might be a tumor.
Ben Larimer's passion is the search for new imaging methods to fight cancer and other diseases.If you don’t get excited talking to Ben Larimer, Ph.D., a researcher developing new imaging tests in the UAB Department of Radiology, you might be a tumor.
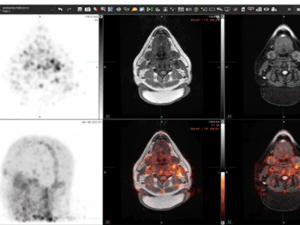
Anyone else would have a hard time resisting Larimer’s vision for a new way to visualize the life-and-death battle between cancer cells and T cells, the immune system’s assault team. Developed while Larimer was at Harvard Medical School — and set to go into human clinical trials this fall in Boston and at UAB — GZP is a new type of PET scan. In a series of papers, including one published this year in the journal Clinical Cancer Research, Larimer and colleagues demonstrate the way GZP can capture images of the immune system’s T cells delivering a knockout punch to tumors — or just milling around, not doing much of anything.
Either way, doctors can find out in days, rather than weeks or months, how a patient is responding to powerful immunotherapy drugs known as checkpoint inhibitors. If the immune system is active, the drug is working; if not, it’s time to try something else. That’s important, because checkpoint inhibitors are like Longfellow’s little girl: when they are good, they are very, very good, but when they are bad they are horrid.
Cure — or nothing — or worse
“Cancer immunotherapy has changed cancer treatment in the past five to 10 years,” said Larimer, who is an associate scientist at the O’Neal Comprehensive Cancer Center at UAB. “You can get cures, or what appear to be cures.” For decades, researchers have known that the immune system is capable of destroying cancer cells, as long as the cancer cells don’t find a way to turn it off first. “And tumors are really good at turning it off” using the immune system’s own safety checkpoints, Larimer said. Checkpoint inhibitor drugs override those systems and “take the brakes off.” That lets effector T cells move in for the kill, a blow they deliver by releasing granzyme B, a powerful enzyme that induces cell suicide.

That’s what happens in some cases, that is. Unfortunately, “the reality is that for most patients it’s not going to work,” Larimer said, with response rates anywhere between 5 and 60 percent depending on the tumor and drug — or drug combination — used. Immunotherapy is “often associated with severe immune-related adverse events, including, hepatitis, colitis and even death, with grade III/IV [that is, severe to life-threatening] adverse events occurring in up to 50% of patients on PD-1/CTLA-4 inhibitor combination regimens,” as Larimer and colleagues pointed out in the introduction to this 2017 paper.
“And the traditional metrics we use for response — tumor size and longevity — are not good at telling you if a therapy is working in a timely manner,” Larimer said.
Can we even do that?
That reality spurred the work that led to GZP, which “can essentially detect when your immune system is killing your cancer,” Larimer said. “We do that by visualizing the enzyme that actually kills the cells,” which is quite a trick. Larimer himself wasn’t sure if it would ever work.
PET imaging relies on chemically binding a target — some naturally occurring substance in the body — to a radioactive tracer (in this case, gallium Ga 68-GZP) that is visible to the PET scanner’s cameras.
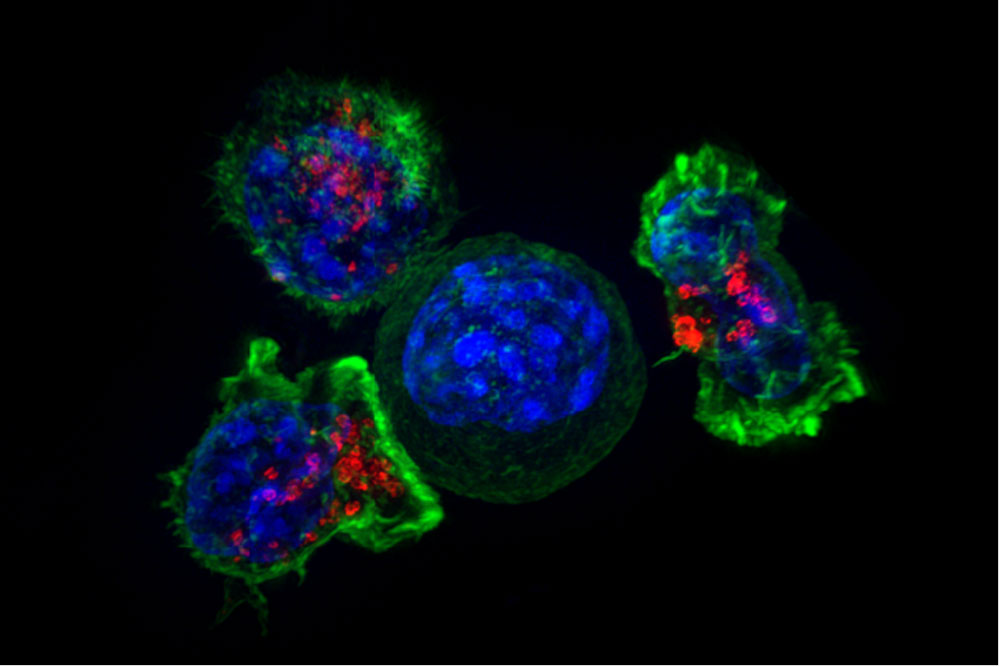
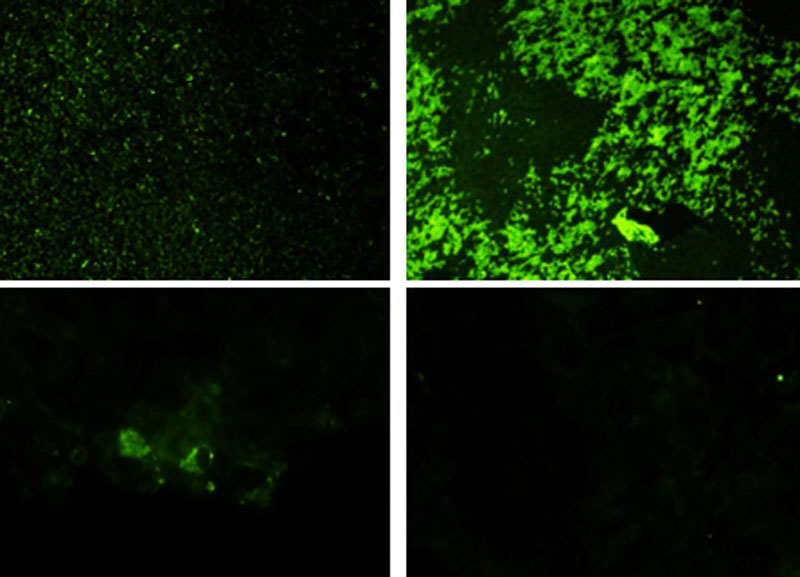 In these enlarged images from Larimer's lab, levels of granzyme B (green) are demonstrably higher in human melanoma samples for responders to various immunotherapy drugs (top) compared with non-responders (bottom).
In these enlarged images from Larimer's lab, levels of granzyme B (green) are demonstrably higher in human melanoma samples for responders to various immunotherapy drugs (top) compared with non-responders (bottom).
Granzyme B is carried about in vesicles inside T cells. “When you’re making an imaging agent you want it to target a cell-surface receptor, which granzyme B is not,” Larimer said. “We had a lot of debates whether it was even possible to target it. Granzyme B is so toxic that at the time people didn’t even make it in a pure and active form we could use in the lab.” On the day the lab finalized its first experiment in animal models, “we looked at the data and I saw one of the tumors was just glowing,” Larimer recalled. “I texted the guy I was working with and said, ‘You’re never going to believe this — it worked!’”
The results started to accumulate. “We tested it in animal models, and we were able to predict with a high degree of accuracy which ones would respond and which ones would not respond,” Larimer said. “We did human samples, and they looked the same. So we spun out a company based on that in order to get clinical trials going quickly.” (Academic research labs are not equipped or funded to make patient-ready treatments. That’s why UAB launched the Alabama Drug Discovery Alliance with partner Southern Research, to give promising UAB discoveries the best chance to reach the clinic. Read more in this UAB Magazine story.)
Not ‘Who gets credit?’ but ‘How can I help?’
At the same time, Larimer, who was still a postdoctoral fellow, was looking for a faculty position — somewhere where he could fulfill his “passion, which has always been developing new tracers,” Larimer said. At conferences, Larimer had met Suzanne Lapi, Ph.D., who is vice chair of translational research in the Department of Radiology, director of UAB’s Cyclotron Facility and director of the Division of Advanced Medical Imaging Research, and Jonathan McConathy, M.D., Ph.D., associate professor of radiology, director of the Advanced Imaging Facility and director of the Division of Molecular Imaging and Therapeutics. The O’Neal Comprehensive Cancer Center at UAB, which houses the Cyclotron and Advanced Imaging facilities, had a faculty opening, “so they brought me down,” Larimer recalled. “I was blown away. The facilities here are as good or better than the traditional top-tier places” for medical imaging research.
Everyone wants to work with the latest technology in their field. The Cyclotron Facility’s layout, with PET scanner, cyclotron and patient rooms only steps apart, and all a short elevator ride from his Cancer Center lab and office, is a “very helpful physical blueprint,” Larimer said. “But it’s as much the people as it is the physical tools. The culture of the department and the collaborative environment at UAB is really refreshing. People really support research here, which is important for a hospital-based setting. They’re not trying to keep things for themselves. The first question when you have a new idea is not, ‘Who gets credit for it?’ but ‘How can I help?’ And that is contagious. It makes every day fun.”
Clinical trial on the way
The company Larimer co-founded, Cytosite Biopharma, already was moving toward a clinical trial in Boston, but “once I accepted the offer to come to Birmingham, I realized we should be doing this at UAB” also, Larimer said. “We have everything we need here, all in one place. UAB will either be the first or second site in the world to be doing granzyme B imaging.” The clinical trial, which will, like all early-stage human trials, focus on safety initially, plans to enroll patients with melanoma and lung cancer and launch this fall, Larimer said.
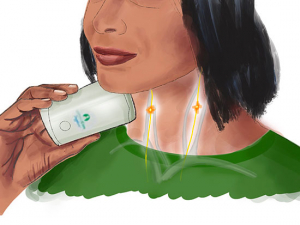
“The idea is after the first round of therapy and before the second round, patients will come in and get scanned with this imaging agent,” Larimer said. “If there’s a high signal in your tumor, that means the immune system is actively killing the tumor. If not, your immune system is not activated.” This indication of ineffectiveness also mean patients who aren’t being helped could stop taking a drug before they experience the side-effects, which “typically occur after the third or fourth cycle,” Larimer said. “The goal is to have this eventually become part of an oncologist’s toolbox.”
Get it quick
One of the most important elements on the new-tracer checklist is its half-life — how long it takes for half of the generated substance to revert to its previous state. (A cyclotron makes radioactive tracers by bombarding a target with protons. See how it works in this feature.) If it’s too slow, the patient is subjected to unnecessary radiation exposure. Too fast and the tracer won’t reach the place in the body you want before it’s all gone. The half-life for the GZP peptide is 20-30 minutes, Larimer said. “It is injected and one hour later the patient is scanned” in a PET machine, he said. “Five hours later there is no trace of the imaging agent left in the body.”
| “We can essentially detect when your immune system is killing your cancer. We do that by visualizing the enzyme that actually kills the cells.” |
At UAB, the peptide will be synthesized in the Cyclotron Facility and delivered directly to a patient room next door. The patient then walks down the hall a few dozen feet to the PET scanner in the Advanced Imaging Facility. “When I offered UAB as a second trial site, people were really excited about the setup here.”
What stops the killers?
There is a giant question remaining, of course: Why do some people respond to immunotherapy and others don’t?
“That is the hottest area of research now,” Larimer said. “In mice it looks like it’s dependent on which type of cancer it is. If it’s a really aggressive tumor totally driven by T-cell activation, for example.” And that could essentially be random. “Does a regulatory T cell get there before an effector T cell?” Larimer said. “It’s not decidedly known at this point.” Larimer’s lab is using granzyme B to identify tumor tissue with high response and low response, so they can be better characterized. “That’s our approach to using granzyme B imaging to contribute to the biology of this.”