|
Diagnosis: Echinococcus granulosus. Complicated multivesicular liver hydatid cyst with intrabiliary rupture and cholangitis.

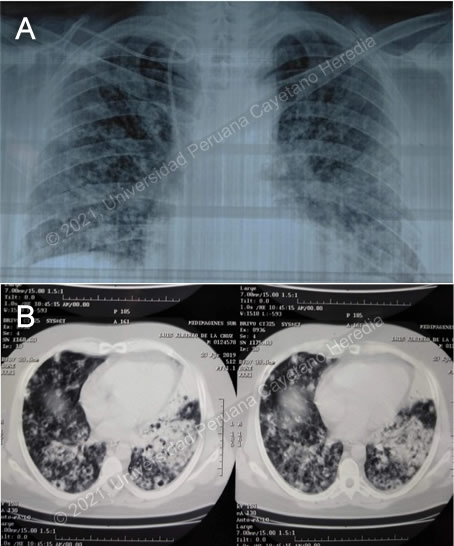
Discussion: After the procedure an abdominal CT scan was taken (Image 2), which shows two cystic lesions in the liver with a heterogeneous content; the larger one has daughter cysts inside.
The patient was treated with broad spectrum antibiotics and albendazole for 4 weeks and scheduled for surgery.
A laparoscopic left hepatectomy was performed, a large cyst was observed broken into the biliary tract at four different points. The fistulas were sutured and a capitonage and closure with omentum were performed. The patient did not have an allergic reaction with the rupture of the cyst.
Liver hydatid cyst rupture is classified into three types: a) contained rupture, when the endocyst (acellular multilaminated membrane and nucleated internal germinal membrane) ruptures but the content is confined within the pericyst (compressed host organ parenchyma), b) communicating rupture, when cyst content escapes usually into the biliary tract because the pericyst incorporates biliary branches as it expands, and c) direct rupture when both endocyst and pericyst tear and the full content spills into the abdominal cavity (AJR 1988;150:1051-3). When the cyst communicates with the biliary tract it may involve the common hepatic duct, lobar branches or small intrahepatic branches, the latter are most commonly involved. Small communications between liver cysts and the biliary tree seem to be common (40-90%) and are usually asymptomatic, but large tears are less frequent (5-10% of these) causing biliary tree obstruction and potentially serious complications such as cholangitis, hepatic abscesses, acute cholecystitis, acute pancreatitis and even biliary cirrhosis (Br J Surg 1971;58:228-32; AJR 1982;139:699-702). CT can help identifying the communication between the liver cyst and the biliary tract by showing the defect or discontinuation of the cyst or indirectly by showing linear and irregular tracts inside the biliary tract. Multidetector CT enhances the view of the common bile duct and may be used as an adjunct diagnostic technique in cases of suspected major tears into the biliary tract (Abdom Imaging 2011;36:433-7). ERCP may be used to remove the contents of the cyst, as in this case, but usually surgical exploration is needed.
Human hydatid disease secondary to Echinococcus granulosus is caused by the larval form of this dog tapeworm. Humans ingest the tapeworm eggs in environments contaminated by canine feces and become accidental intermediate hosts. Sheep are the normal intermediate hosts. In general, disease is diagnosed in adulthood as larval cysts expand slowly over years or decades, becoming symptomatic as they impinge on other structures by virtue of their size. The cysts contain hundreds of viable protoscolices capable of becoming adult tapeworms upon ingestion by a definitive host such as the dog. The cyst wall is composed of a 1 mm thick acellular multilaminated membrane, followed by the nucleated internal germinal membrane that is about 0.1 mm thick. The internal germinal membrane lining the cyst produces new protoscolices on an ongoing basis and may also give rise to daughter cysts inside the original cyst. Each protoscolex is capable of becoming a new daughter cyst should the original cyst rupture or be ruptured.
Cystic hydatid disease due to E. granulosus is common in sheep and cattle raising areas worldwide. Most primary infections involve a single cyst. In adults, 65% of solitary cysts are found in liver, 25% in lung and the rest in a wide variety of other organs including kidney, spleen, heart, bone and brain. In patients with a pulmonary cyst, approximately 18% will also have a hepatic cyst.
The majority of patients with hydatid cysts have no or mild eosinophilia. This patient had near to hypereosinophilia (1483 eos/uL). Eosinophilia may occur in asymptomatic patients but is more common after surgery or when the cyst ruptures, as in this case. The cyst with the daughter cysts had ruptured into the biliary tract but not into the peritoneal cavity, so there was no intraabdominal seeding of the cyst contents; during surgery there was also no obvious intraperitoneal seeding. Cysts opened to the biliary tree, bronchi, abdominal cavity or urinary tract should be treated surgically, praziquantel (a very effective protoscolicidal agent) or albendazole is given postsurgically in case there was any inadvertent secondary seeding.
The finding of characteristic cysts and membranes in the main duct was diagnostic, so there was no need for doing a serology, which may be negative in intact cysts.
Albendazole was given for four weeks prior to surgery, presumably trying to sterilize the cyst before surgery. The presence of daughter cysts decreases the effectiveness of this measure. One of the concerns is the use of albendazole in a patient with elevated transaminases, because it is one of its side effects in addition to leukopenia. In this case the elevated transaminases were most likely due to the cholangitis, and albendazole administration was apparently well tolerated.
The patient was referred to us because he was found to have a remaining liver cyst of less than 3 cm in diameter. In his laboratory tests, the eosinophil count was 230/uL and ALT was 17 U/L. He started medical therapy with albendazole. Response of small cysts to albendazole is usually good.
|