In fiscal year 2019, UAB researchers received a record $602 million in grants and contracts, marking a second year of double-digit percentage growth in funding. That productivity has carried on unabated in 2020, and you can follow along. Every Tuesday, Research Administration releases a list of the grants and contracts awarded the previous week (BlazerID required).
In this new series, we’re spotlighting new or re-funded projects to offer a window into the groundbreaking, lifesaving work done by our colleagues around campus. (See other stories in this series, profiling grants to accelerate HIV suppression, test a new strategy against lupus, stop online opioid sales and build freezers for the International Space Station.)
This week, we’re taking a look at an effort to take on the most feared complication of new blood thinners: hemorrhage, or uncontrolled bleeding.
Project title: Predictors of Hemorrhage among Patients on Direct Acting Oral Anticoagulants
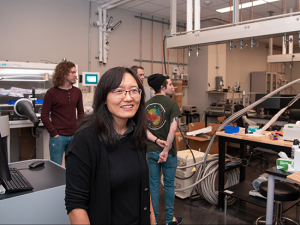
Principal investigator: Nita Limdi, PharmD, Ph.D., professor, Department of Neurology, associate director of Pharmacogenomics, UAB Hugh Kaul Precision Medicine Institute; co-investigators: Mark Beasley, Ph.D., Department of Biostatistics; Todd Brown, M.D., Division of Cardiovascular Disease; Michael Allon, M.D., Division of Nephrology; and Thomas Nolin, PharmD, Ph.D., University of Pittsburgh.
Funding: Five years, $3.68 million from the National Heart, Lung and Blood Institute
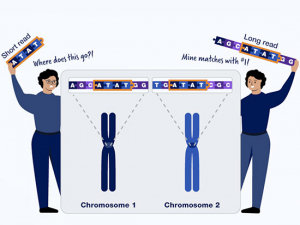
 Atrial fibrillation, the most common heart rhythm disorder, is treated with anticoagulant "blood thinning" drugs to prevent clots that lead to strokes. But these drugs also carry a risk of hemorrhage. UAB researchers are studying the effects of a widely used class of anticoagulants to develop personalized prescriptions to match the ideal dose for each patient.During the past 15 years, Limdi and colleagues have identified clinical and genetic factors that account for response to anticoagulant and antiplatelet therapies. These blood-thinning drugs, including warfarin (Coumadin) and clopidogrel (Plavix), are widely used to prevent clotting in patients at risk for stroke, atrial fibrillation and other conditions. Among other findings, the investigators have demonstrated that race influences the dose requirements for warfarin, and a simple genetic test to determine a patient’s response to clopidogrel can significantly reduce the risk of cardiovascular events in patients receiving a heart stent.
Atrial fibrillation, the most common heart rhythm disorder, is treated with anticoagulant "blood thinning" drugs to prevent clots that lead to strokes. But these drugs also carry a risk of hemorrhage. UAB researchers are studying the effects of a widely used class of anticoagulants to develop personalized prescriptions to match the ideal dose for each patient.During the past 15 years, Limdi and colleagues have identified clinical and genetic factors that account for response to anticoagulant and antiplatelet therapies. These blood-thinning drugs, including warfarin (Coumadin) and clopidogrel (Plavix), are widely used to prevent clotting in patients at risk for stroke, atrial fibrillation and other conditions. Among other findings, the investigators have demonstrated that race influences the dose requirements for warfarin, and a simple genetic test to determine a patient’s response to clopidogrel can significantly reduce the risk of cardiovascular events in patients receiving a heart stent.
While anticoagulation research, including clinical trials, primarily has been conducted in patients of European descent, Limdi has leveraged the patient diversity at UAB to understand differences in anticoagulation response by race, making important contributions to understanding racial differences — and the underlying factors behind those differences — in drug response. “The population served at UAB and the research infrastructure here have provided unique attributes that have been vital to the success of our efforts in pharmacogenomics,” Limdi said.
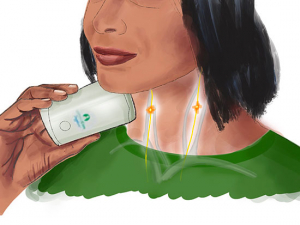
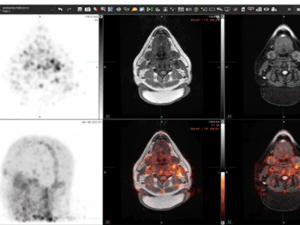
With this new NHLBI grant, the researchers will focus on two challenging issues related to the most commonly used direct-acting oral anticoagulant (DOAC) drugs, rivaroxaban (Xarelto) and apixaban (Eliquis). These newer therapies “are now preferentially used over warfarin,” Limdi explained. However, it is not clear what precise dosages are needed to avoid hemorrhage — “the most feared complication of anticoagulant therapy,” Limdi said — and take patients’ kidney function into account. The funding will allow Limdi and colleagues to conduct the largest study of its type to analyze the relationship between DOAC dosing, DOAC levels in the blood and anticoagulation intensity across the spectrum of kidney function.
| While anticoagulation research, including clinical trials, has been mainly conducted in patients of European descent, Limdi has leveraged the patient diversity at UAB to understand differences in anticoagulation response by race. |
The grant also will create a prospective cohort of thousands of atrial fibrillation patients treated with Xarelto and Eliquis. The aim is to develop clinical prediction rules that will enable physicians to make a patient-specific risk-benefit assessment before prescribing these medications. “It will enable personalized choice for oral anticoagulant therapy,” Limdi said. Genomic DNA from participants also will be used to identify novel genetic variants associated with hemorrhage.
The work has immense potential, as the burden of atrial fibrillation continues to increase in the United States and around the world, Limdi said. Between 1990 and 2013, the global prevalence of a-fib, the most common heart rhythm disorder, rose by 63 percent. Aging populations worldwide mean the prevalence is expected to double again, to 12.1 million cases in 2030, and to approach 18 million in Europe by 2060, reaching epidemic levels.
“Identification of factors that predict risk of hemorrhage among patients taking DOACs is vital as it can help identify patients who stand to benefit or be harmed by anticoagulant drugs,” Limdi said. “The integration of these predictors into the current treatment approach can help provide personalized treatment and improved outcomes for individual patients.”