Department welcomes new staff members

Andrea Boohaker, MSN, ACNP-BC, RNFA - APP team lead
Andrea Boohaker joins the department as APP team lead for the Departments of Neurosurgery and Orthopaedic surgery. Andrea earned her MS degree in nursing from Vanderbilt University in 2007 and is currently enrolled in the UAB Doctor of Nursing Practice program, she will graduate in Dec. 2021. She has worked as an orthopaedic trauma nurse practitioner for over 14 years and began her career at the University of Texas (UT) at Houston. During her time at UT Houston, she developed a passion for increasing autonomy for advanced practice providers and improving the overall quality of training. Andrea serves on the Ambulatory Access Executive Committee and the Provider Practice Optimization Steering Committee at UAB, representing the advanced practice cohort. She also serves as a clinical instructor in the graduate program at UAB School of Nursing. Andrea is a Sigma Theta Tau Nursing Honor Society member and was recently awarded the UAB Medicine Excellence Award for 2021.

Casey Lee, RN
Casey Lee joins the department as a registered nurse. Originally from Meridian, MS, Casey graduated from the University of Alabama in 2009 with a bachelor’s degree in business but decided to change careers shortly thereafter. She received her associate degree in nursing from Jefferson State Community College in 2012. Since, she has worked at Children’s of Alabama, beginning as a clinical assistant and continuing as a nurse in Med-Surg and Surgical Services. She looks forward to joining the pediatric neurosurgery team, where she will function as the nurse clinician for Dr. Brandon Rocque.

Dana Belmont - Administrative office specialist
Dana joins the department as an administrative office specialist. Originally from Buffalo, NY, Dana moved to Birmingham in 2014 after traveling the world with the military and family. She began working for the UAB Department of Medicine in 2014 and joined the Department of Neurosurgery in 2016, where she was the clinic coordinator at Greystone. In October 2020, she moved to Raleigh, NC for a short time before returning to Birmingham. Dana is excited about her new journey in neurosurgery.

Kirsten Yelvington, MS - Operations Administrator
Kirsten joins the department as operations administrator. Originally born in Colorado, Kirsten grew up in several areas in Europe and across the U.S. Her healthcare career began over 20 years ago at UF Health in Gainesville, FL as a neurodiagnostic technologist. After, she moved to Pensacola, FL, and worked at HCA West Florida Hospital as coordinator of the EMU and Duke University Hospital as a technical advisor. Since she has been at Mayo Clinic for the past 10 years working in the Department of Neurology. During that time, she earned her bachelor's and master's degrees, was appointed to instructor of neurology and participated in research involving epilepsy and awake craniotomies. In addition, she managed the procedures EEG lab and Level IV Epilepsy Monitoring Unit and facilitated improvement projects that resulted in national accreditation, improved access, and increased volumes.
 Thomas Dillard - MSHA Student
Thomas Dillard - MSHA Student
Thomas Dillard joins the department as an MSHA student. Born and raised in Birmingham, AL, Thomas graduated from the University of Montevallo in 2021 with a bachelor's of business administration in management degree. He is currently pursuing his master's of science in health administration at UAB. Thomas worked closely with higher education administrators in his undergraduate career as an administrative assistant within the University President's Office. He was also elected as the Student Government Association President in 2020 and served on the University of Montevallo COVID-19 Task Force as a representative of the student body. Thomas looks forward to joining the Department of Neurosurgery, where he will primarily work with Donna Bailer.
Bailer named president-elect of NERVES
 Department of Neurosurgery Executive Administrator Donna Bailer, J.D., LL.M., was elected president-elect of the national Neurosurgery Executives’ Resource Value and Education Society (NERVES) at its annual membership meeting in September 2021.
Department of Neurosurgery Executive Administrator Donna Bailer, J.D., LL.M., was elected president-elect of the national Neurosurgery Executives’ Resource Value and Education Society (NERVES) at its annual membership meeting in September 2021.
Staner featured in UAB MedCast Podcast
 UAB Department of Neurosurgery Clinical Professor Thomas Staner, M.D., FACS, was a recent guest on UAB MedCast - a medical education podcast for healthcare professionals. He joins a long list of experts to speak on various topics and innovations in the field of healthcare.
UAB Department of Neurosurgery Clinical Professor Thomas Staner, M.D., FACS, was a recent guest on UAB MedCast - a medical education podcast for healthcare professionals. He joins a long list of experts to speak on various topics and innovations in the field of healthcare.
Resident Spotlight: Dr. Arsalaan Salehani
 Dr. Arsalaan Salehani is a PGY-6 in the Department of Neurosurgery.
Dr. Arsalaan Salehani is a PGY-6 in the Department of Neurosurgery.
Hall named department wellness champion
 The Department of Neurosurgery has selected Shannon Hall, CRNP, to serve as wellness champion through the UAB School of Medicine (SOM) Office of Wellness.
The Department of Neurosurgery has selected Shannon Hall, CRNP, to serve as wellness champion through the UAB School of Medicine (SOM) Office of Wellness.
Department celebrates Women in Medicine Month
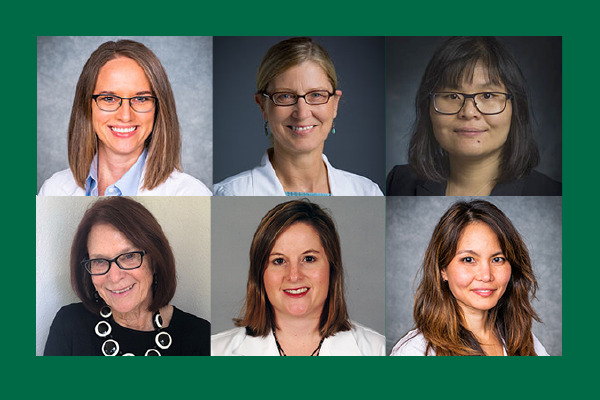
Top (L to R): Drs. Nicole Bentley, Melissa Chambers, Jianmei Leavenworth, Bottom (L to R): Beverly Walters, Kristen Riley and Elizabeth Liptrap
The Department of Neurosurgery would like to recognize the month of September as Women in Medicine Month.
The Association of American Medical Colleges (AAMC) created Women in Medicine Month to recognize the growing number of women in the profession. The month-long observance celebrates women in educator, scientist, leadership, and physician roles.
According to the National Institutes of Health, women represent only 12 percent of neurosurgeons in the United States. At the UAB Department of Neurosurgery, women make up 25 percent of the overall faculty and 21 percent of the clinical neurosurgeons. This is due to reaffirming efforts aimed to increase diversity within the university and the UAB Health System.
“Surgery in general, and neurosurgery in particular, have long been male-dominated specialties,” said James Markert, M.D., Ph.D., professor and chair. “Commitment to diversity is a cornerstone of UAB, and we feel that our entire department, from faculty to trainees, as well as our patients, are well served by a diverse workforce.”
Learn more about our physicians
Adjunct Professor
Assistant Professor
Assistant Professor
Professor
Professor
Associate Professor
Spotlight
Drs. Elizabeth Liptrap and Kristen Riley discuss life outside of work, what inspired them to become neurosurgeons, and their proudest accomplishment.
-
Elizabeth Liptrap, M.D.
Life outside of work
I am originally from Maryland but moved here two years ago to work at UAB. I am so proud to be a part of the UAB Department of Neurosurgery and love living in Alabama. My husband works in real estate and the Air National Guard. We love spending time with our family, anything outdoors, country music and dogs. We are excited about our baby girl arriving in November.
What do you enjoy most about your career?
I am still early in my career, but my favorite things are still preparing for and performing procedures, helping patients navigate through decisions about their care and working with residents/fellows.
What inspired you to become a neurosurgeon?
I initially chose to become a neurosurgeon because I enjoyed the complexity of cases and significant potential to contribute to the field, particularly in neuro-oncology and cerebrovascular surgery. My father was diagnosed with a GBM when I was a PGY-6 and going through that experience from a patient and patient’s family perspective increased my passion for and dedication to the field of Neurosurgery.
What is your proudest accomplishment?
Any time a patient and/or family is happy with their care is the greatest reward for me.
-
Kristen Riley, M.D.
Life outside of work
I am married with two boys (ages 16 and 20), and we have two dogs! I am a huge sports fan and enjoy attending sporting events. One of my bucket list items is to visit all MLB and NFL stadiums.
What inspired you to become a neurosurgeon?
I originally thought I would be an orthopaedic surgeon, but everything changed during my third year of medical school when I was exposed to neurosurgery. I was hooked!
What is your proudest accomplishment?
Having a great team that provides quality compassionate care to our patients.
-
Nicole Bentley, M.D.
Life outside of work
I am married with 2 kids (5 yo and 10-month old). We stay very busy! We love to cook together, be outdoors, and travel as much as COVID will allow.
What do you love most about your career?
I love that in my subspecialty of functional neurosurgery, we have the opportunity to make significant impacts on patients’ quality of life, helping them to gain more enjoyment in their day-to-day activities. I also love that the field of neuromodulation is growing as we learn more about how the brain works at a fundamental level.
What is your proudest accomplishment?
My family!
The department welcomes new staff members

Eva Gilliam - administrative assistant
Eva Gilliam joins the department as administrative assistant. Gilliam will spearhead organizational tasks and assist department executive administrator, Donna Bailer. Previously, she dedicated 25 years of service to UAB in areas including pediatric orthopaedics, epidemiology, radiology and nutrition sciences. Following, she moved to Gainesville, Florida, to help Community Health Services with their mission in reducing homelessness among individuals suffering from drug addiction and mental illness. Since, she has returned to Birmingham to reunite with her family. “Everyone in Neurosurgery has been so welcoming and helpful. I have enjoyed my first two weeks and am looking forward to becoming more confident in my new role.” Said Gilliam.

Tori Caudill - research coordinator II
Tori Caudill joins the department as research coordinator II for pediatric neurosurgery. She graduated from UAB with a Bachelor’s of Science in Psychology and Neuroscience in 2019. Caudill has spent the last few years as a research assistant in various departments including nephrology and pediatric oncology. She loves developing research questions, assisting with research design, presenting research, and learning about the brain (especially in relation to behavior and psychology). She plans to pursue her Ph.D. in behavioral neuroscience.

Cameron Roby - healthcare management intern
Cameron Robby joins the department as a healthcare management intern. Originally from Warner Robbins, Georgia, Robby moved to Birmingham two years ago to pursue the healthcare management program at UAB. In addition, Robby will also work as a secretary in the UAB Trauma Burn Nursing Unit. In her free time, she enjoys working out, playing volleyball, video games, and baking.
Johnston and Leavenworth promoted
 The UAB Department of Neurosurgery is pleased to announce the promotion of Associate Professor James Johnston, M.D., and Assistant Professor Jianmei Leavenworth, M.D., Ph.D., effective October 1. Listed below are their promotions.
The UAB Department of Neurosurgery is pleased to announce the promotion of Associate Professor James Johnston, M.D., and Assistant Professor Jianmei Leavenworth, M.D., Ph.D., effective October 1. Listed below are their promotions.
Read more
Pediatric Fellow Spotlight: Dr. Arianna Barkley

Arianna Barkley, M.D., joined the Department of Neurosurgery this summer as a pediatric fellow.
Read moreJones guest on UAB MedCast, discusses HHT
 UAB Department of Neurosurgery Assistant Professor Jesse Jones, M.D., was a recent guest on UAB MedCast - a medical education podcast for healthcare professionals. He joins a long list of experts to speak on various topics and innovations in the field of healthcare.
UAB Department of Neurosurgery Assistant Professor Jesse Jones, M.D., was a recent guest on UAB MedCast - a medical education podcast for healthcare professionals. He joins a long list of experts to speak on various topics and innovations in the field of healthcare.
Spain Rehab Honors Patient for Building a Better Quality of Life

Mark McColl, chairman of Lakeshore Foundation and a longtime patient of UAB Spain Rehabilitation Center (SRC), is the 2020 recipient of SRC’s Ambassador of Hope Award.
The annual award goes to a disabled individual whose courage and determination inspire hope in others who face the challenges of disability.
McColl, 61, is a native of Chattanooga, Tenn., and a graduate of the University of Alabama. He began a successful career in engineering in the 1980s, starting in Houston and ending up in Birmingham, where he eventually took a position with Rust Engineering. It was there that McColl earned such accolades as ISA Young Engineer of the Year in 1988 and Rust Engineer of the Year in 1990. In 1995 he started his own company, Process Automation and Simulation Services (PASS), which grew to more than 50 employees at its peak before McColl retired in 2011.
It was not the early retirement he wanted. It was instead the inevitable result of McColl’s decades-long journey with a spinal cord injury that, over time, robbed him of much of his mobility.
“I didn’t have the typical sudden, acute spinal cord injury,” McColl says. “It was a disc rupture that slowly developed. In 2000, I began losing sensation in my left leg and having weakness in my right. Since I wasn’t having any problems with my arms or hands, my doctor assumed that I had problems in the lumbar region. He ordered imaging of that area and put me in physical therapy. By the time I began to lose use of my right leg, additional imaging showed that I had a severe cervical rupture.”
His condition was the first stage of spine deterioration and led to years of surgeries and treatments. The first surgery was a removal of the ruptured disc and a fusion of his C6 and C7 vertebrae, but as weakness in McColl’s legs increased and bladder problems emerged, he sought care from UAB Medicine neurosurgeon Mark Hadley, MD. In 2001, McColl underwent surgery to redo the fusion of the cervical vertebrae, which had failed.
McColl began doing outpatient physical therapy at Lakeshore Rehabilitation Hospital in 2003 and then joined the Lakeshore Foundation in 2004 to continue therapy. Weakness in his legs and right side progressed, so he sought treatment at multiple medical centers around the country. By 2007, McColl still had no answers for why he continued to lose sensation and function, other than the original damage to his cervical cord.
Full-Time Struggle
At that time, McColl was still managing the engineering firm he had started in 1995. “By 2009 I could barely walk, initially requiring one cane and then two, and I was limited to short distances, he says. “At the same time I was staying in good shape through physical therapy.”
As an engineer interested in new technologies, at each stage of loss McColl would find new devices that allowed him to remain as active as possible. He began using a Segway, a two-wheeled, self-balancing personal transportation device that seemed ideal for his needs, as he could ride it long distances and then use his canes for the final few steps. Soon after that adaptation, he began needing crutches to move short distances. In late 2010, McColl retired from the firm he founded to pursue what he calls a “last-ditch effort” to stay out of a wheelchair. He would tell people that his new job was now “full-time physical therapy.”
McColl traveled to Germany in 2011, where a surgeon replaced his L4/L5 disc with an artificial disc. A year later, follow-up imaging revealed that the section required fixation, which is a procedure used to internally set and stabilize fractured bones.
“It was one of the toughest things I had ever gone through,” he says. “I really didn’t think I could endure a second round of that, with the surgery, recovery, and travel being so grueling.”
Instead, McColl returned to UAB Medicine to again receive care from Dr. Hadley, who performed the lumbar fixation. The surgery was successful, but it hastened McColl’s inevitable decline to a wheelchair and a bladder and bowel program.
“At that point, I caught a major break in my journey,” McColl says. “My three weeks as an inpatient at Spain Rehab were under the care of Reid Warren and Alex York, a great pairing of physical and occupational therapists who were not reluctant to push me hard. I was lucky to have that team, because I figure if you are going to face the challenge of PT/OT anyway, you may as well go as far as possible. So you need that coaching and pushing on a lot of days when you might not try as hard on your own.”
A Peculiar Positive View
McColl says that a sense of humor, a positive outlook, and a willingness to push his limits are the only ways he has been able to manage his disability. With self-deprecating humor, McColl does note that you have to be careful what you wish for in that respect.
“For my first day of inpatient therapy, I didn’t have my usual therapists, and we were done in an hour,” McColl says. “Being a smart aleck, I asked the PT, ‘Is that all you’ve got?’ I was kidding around, but for her, my remark was the wrong challenge – even as a joke. She continued my therapy for another 30 minutes to show me what a real physical challenge felt like. I found out later that she was a bodybuilder! I tell this story often to show that you can always find humor, even in the midst of medical challenges and setbacks, and also to persuade others that they can go farther than they think they can, given the right circumstances, the right care teams, and a positive frame of mind.”
McColl says he understands that it’s an odd way to look at his situation, but he insists that going into the wheelchair actually improved his quality of life.
“Before that, especially when I was using crutches, just getting around or worrying about going to the bathroom would complicate daily life, to say the least,” he says. “It was painful and socially limiting too, since I was capable of maybe one outing a day. Moving to the wheelchair, along with making the change to catheterization for the bladder issues, made almost everything easier. So my daily focus became rehab at Lakeshore, and the wheelchair changed a lot of that, too.”
McColl says he was spending 3-4 hours at Lakeshore each day, between time in the pool, the fitness center, and playing wheelchair sports such as rugby, football, softball, and tennis.
“By 2014, I had been a member at Lakeshore for 10 years,” McColl says. “I guess they were thinking, ‘We need to get some work out of this guy.’ So in sheer desperation they asked me to be a board member. I was excited because it was a chance for me to give back to the organization that had given me so much.”
A Difficult Setback and New Adventure
In 2016, McColl suddenly faced what he regards as the most difficult period of all. After experiencing new numbness and weakness in his left leg, he underwent surgery to replace the screws and rods that had been placed in his back in 2012 and extend them to L3. The day after surgery, he fractured the L3 vertebra when he twisted to one side. This led to more surgery to extend the screws and rods to L2. Unfortunately, that vertebra fractured less than two weeks later, while McColl was at Spain Rehabilitation Center. This required two additional surgeries, with screws and rods extended all the way to T8.
McColl developed an infection and remained in the hospital for an extended period of time. Then he transferred back to SRC as an inpatient for another three weeks. All told, he was undergoing and recovering from surgeries from early November 2016 until two days before Christmas.
“It was definitely at my lowest point,” McColl says. “I know that because it’s the only time I briefly lapsed into a phase of depression. But you do what you have to do. Undergoing all the procedures and therapies for two full months set me back physically, too. At that point I knew it would be the wise, safe choice to give up wheelchair sports. I began looking for other activities to fill my time.”
Ever the engineer, McColl took an interest in 3D printing, specifically in creating devices for people with disabilities. In 2018, he and another Lakeshore member, Clay Bracket, formed Ability Tech Solutions. The company designs innovative items such as beverage holders and keychain clips that attach to wheelchairs. They also patented an automatic wheelchair lock.
“Most people with disabilities also struggle financially,” McColl says. “We wanted to make affordable items, so that was part of the design challenge. Clay, who has incomplete quadriplegia, and I both see ourselves as ideal designers because we understand the particular needs of people in wheelchairs. My getting involved with 3D printing just shows you that there’s always something out there if you look for it. For me, this experience is the textbook example of, ‘Okay, if this chapter of my life has to end, then what is my new chapter about? What can I accomplish? What’s the next adventure?’”
‘Shortest Path to a Better Life’
In 2017, McColl was approached to become vice-chair of the board of the Lakeshore Foundation, and he became chairman two years later. Another opportunity arose from his relationship with Reid Warren, manager of UAB Medicine Inpatient Rehabilitation Therapy.
“One day I was at Spain Rehab to get an X-ray,” McColl recalls. “I happened to see Reid, and he told me he was interested in getting Spain inpatients to visit Lakeshore Foundation and show them what’s possible. The idea was to let these patients see people like themselves playing sports, being independent, and leading full lives. I told him it was an awesome idea and to let me know what I could do to help make it happen.”
Warren says the patient relationship grew into a friendship. “Mark was one of my most memorable patients,” Warren says. “His infectious optimism and desire to better our community made a lasting impression, and I am grateful for the friendship we’ve maintained through the years. He has been an outstanding leader for Lakeshore Foundation.”
The annual Ambassador of Hope Award is the formal recognition of McColl’s many years of passion and advocacy for Birmingham’s rehabilitation community. He says years of experience with this community have provided him with an important perspective on his own condition.
“One key aspect of my situation is that the physical decline took place over a period of almost two decades,” McColl says. “My slow transition to various stages of disability softened the emotional and mental blows. Many patients I have met at Spain and at Lakeshore experienced a sudden, catastrophic injury that instantly changed their life forever. They had no opportunity to prepare. So I‘m extremely grateful that I have had the luxury of time to adjust. Additionally, I know many, many people who are dealing with much more challenging conditions than I am.”
As for being regarded as an ambassador of hope or a source of inspiration, McColl emphasizes that his approach is that of an engineer who has chosen a specific, logical strategy.
“Maybe it’s the engineer in me talking, but I think a good attitude is just the logical choice,” he says. “Many people credit me with fortitude because I maintain a positive outlook, but by choosing to stay positive, I’m just selecting the shortest path to a better quality of life. It’s a strategy. I’m going to feel better about things, other people hopefully will enjoy being around me, and I can make the most of the time given to me.”
Source: UAB Medicine
Holland named staff diversity liaison
 The Department of Neurosurgery has selected Anastasia Holland to serve as staff diversity liaison to the School of Medicine Office for Diversity and Inclusion (ODI).
The Department of Neurosurgery has selected Anastasia Holland to serve as staff diversity liaison to the School of Medicine Office for Diversity and Inclusion (ODI).
Department of Neurosurgery welcomes Schmalz and Godzik
 L to R: Drs. Philip Schmalz and Jake GodzikThis month, the department welcomed Assistant Professors Philip Schmalz, M.D. and Jakub "Jake" Godzik, M.D.
L to R: Drs. Philip Schmalz and Jake GodzikThis month, the department welcomed Assistant Professors Philip Schmalz, M.D. and Jakub "Jake" Godzik, M.D.
Jones launches EMBOLISE clinical trial to treat subdural hematomas
 Assistant Professor Jesse Jones, M.D., has been tapped by Medtronic to lead UAB in a clinical trial aimed at treating subdural hematomas.
Assistant Professor Jesse Jones, M.D., has been tapped by Medtronic to lead UAB in a clinical trial aimed at treating subdural hematomas.
Resident Spotlight: Dr. Somnath Das

Dr. Somnath Das joined the Department of Neurosurgery this summer as a PGY-1 neurosurgical resident.
Read morePediatric neurosurgery ranks top 50 in the nation
 U.S. News & World Report’s (USNWR) 2021 Top Pediatric Hospital Ranking reported Children’s of Alabama Pediatric Neurology and Neurosurgery specialty 33 in the nation.
U.S. News & World Report’s (USNWR) 2021 Top Pediatric Hospital Ranking reported Children’s of Alabama Pediatric Neurology and Neurosurgery specialty 33 in the nation.
Fisher featured in UAB MedCast
 In part 1 of this series on skull based surgery, Drs. Winfield Fisher and Erika Walsh lead a discussion of the complexity of lateral skull base surgery and the benefit of a team approach. Including discussion of disease processes treated, types of preoperative evaluations, surgical techniques and referral process
In part 1 of this series on skull based surgery, Drs. Winfield Fisher and Erika Walsh lead a discussion of the complexity of lateral skull base surgery and the benefit of a team approach. Including discussion of disease processes treated, types of preoperative evaluations, surgical techniques and referral process
Hello, goodbye 2021: Pediatric Neurosurgery Fellows
More than 1,200 interns, residents and fellows train in every medical specialty at the University of Alabama at Birmingham and at regional campuses in Montgomery, Huntsville, Tuscaloosa and Selma. Each year, a class of trainees graduate and a new class joins UAB, setting off on their trainee experience, whether it be a one-year fellowship program or a seven-year residency.
Read moreResident Spotlight: Dr. Andrew Hale
 Dr. Andrew Hale joined our department this summer as a PGY-1 resident.
Dr. Andrew Hale joined our department this summer as a PGY-1 resident.
Department creates new space for resident wellness and collaboration

The Department of Neurosurgery is pleased to announce the completion of its new resident lounge located on the seventh floor of Jefferson Tower.
Construction began in April and was completed on June 4, 2021. The lounge is outfitted with comfortable seating, desk space and more. Computers, monitors and phones are ordered and will be installed soon.
The goal is to provide residents a space to meet, collaborate, and more importantly serve as a "safe place" where residents can decompress from, at times, the rigorous training they undergo during neurosurgery residency.
"Our residents and their well-being are a top priority of the department. I look forward to seeing the benefits this new lounge will provide to our hard-working trainees," said James Garber Galbraith Endowed Chair of Neurosurgery James Markert, M.D., MPH.
“We are always looking for ways to support our residents and we greatly appreciate their dedication to the program,” said Curtis Rozzelle, M.D., director of the Neurosurgery Residency Program. “Wellness plays a huge role in developing successful neurosurgeons and future leaders in our field .”