By Erica Techo
By Erica Techo
In 2019, a group of Registered Nurse First Assist (RNFA) students joined instructors in the University of Birmingham at Alabama School of Nursing’s simulation lab. They gathered around their skills stations, each equipped with an animal cadaver model, and practiced suturing and learned sterile techniques.
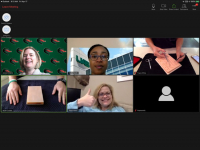
This annual intensive looked a little different in 2020, as intensives moved to remote learning in order to ensure social distancing and minimize the spread of the novel coronavirus (COVID-19). Faculty worked diligently to transition the simulation, originally scheduled for March 25 on campus, to a virtual format by utilizing webcams, review materials and pre-existing skills videos.
“Each student already had a suture kit to practice skills at home, and a big part of this simulation is learning how to suture and tie knots,” said Assistant Professor Tracie White, DNP, CRNP, ACNP-BC, CNOR, CRNFA. “To adapt to a virtual intensive, one of the most important things we did was angled our cameras to focus on our hands during the demonstrations of these techniques.”
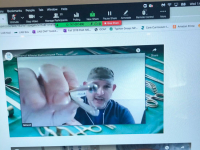
Then, students followed suit and angled their cameras to show their hands while they practiced techniques and received real-time feedback. They later submitted recorded videos of their suturing and instructors provided individual feedback to ensure students mastered the skills.
The transition had its challenges, said Adjunct Clinical Instructor Steve Parsons, MSN, RN, CNL, CNOR, CRNFA, but collaboration with the Office of Instructional Technology and interactive features kept students engaged while providing a fun and educational experience.
“We wanted students to get as much tactile experience as they could, but we couldn’t go so far as to send them the animal cadaver models,” Parsons said, “By incorporating existing videos from the class, showing techniques and explaining suturing step-by-step, we were able to keep everyone engaged and active.”
Parsons said faculty also utilized household resources — including his kitchen sink — to demonstrate a proper surgical scrub.
“Like many concepts when learning sterile technique, a proper surgical scrub is about practicing and muscle memory,” White said. “They can read about it but going through the motions is what makes the difference. This way, students could see the process and know how to practice a surgical scrub at home.”
“The adjustments took a lot of innovative ideas,” Parsons added. “As we discussed gowning and safety steps, we encouraged students to use what they have on hand — bathrobes or kitchen gloves, household items like that.”
The intensive also included guest speakers. Daniel Estille, BSN, RNFA, CNOR, and Minesh Patel, BSN, CRNFA, CNOR, joined via Zoom from an operating room at UAB Hospital. They showed surgical instruments, demonstrated their function and provided examples of their use in surgery. Jared White, MD, FAACS, Surgical Director of the Liver Transplant Program at the Medical University of South Carolina, joined to provide a surgeon’s perspective on the RNFA role, and Lauren Boudreaux, MSN, CRNP, AGACNP-BC, CRNFA, CNOR, who is an RNFA in the Division of Gastrointestinal Surgery at UAB, discussed her career path and offered advice as a former student in this program.
“What I’ve heard from students — our nurse practitioner students in general and for this intensive — is that they realize that we care and are still putting 100 percent into our instruction,” White said. “We are working to give them relevant learning experiences in what is an unprecedented situation. I’m also so impressed with how our students have adapted. Many of them are critical care nurses, and they are working on the front lines, still reporting to class, turning in assignments and taking care of their families.”
“We missed face-to-face interaction with our students, but technology helped provide the best experience possible considering the current circumstances,” Parsons added.