By Laura Gasque and Pareasa Rahimi
Preparing the next generation of nurse leaders requires innovation in all aspects of education, research and clinical practice. The UAB School of Nursing has laid out its goals to elevate its track record of excellence in shaping the future of health care over its more than 70-year history in a new strategic plan for 2024 through 2028—Boldy Blazing Forward, Elevating Excellence to New Heights. Across its three mission pillars—education, service and research—the School is setting a course to further position itself as a global leader by synergizing all the opportunities created within its missions to shape equitable, patient-centered health care and expand the School’s impact.
“It’s no secret that our School is a high-performing organization,” said Dean and Fay B. Ireland Endowed Chair Maria R. Shirey, PhD, MBA, RN, NEA-BC, ANEF, FACHE, FNAP, FAAN. “We are ready to move to the next level of excellence, leveraging our leadership and resources to propel us into the future. We are in an outstanding position to remain strong as long as we stay vigilant, do not rest on our laurels and are strategic in building capacity and seizing opportunities.”
Building faculty capacity
Faculty development is key in building capacity for the future, Shirey said.
The School recently established a Faculty Academy to promote excellence in teaching and provide a strong foundation for faculty development. New faculty teaching in any academic program are required to complete the training during their first year. It addresses topics such as the School’s curriculum framework, methods of teaching and learning, use of technology in the classroom, simulation, excellence in clinical teaching, best practices for promoting student success and retention, and teaching scholarship.

Building skills for innovation to drive change in educational and clinical settings is the goal of the School’s Innovation Fellows, launched in 2023 by the Office of Technology and Innovation. The inaugural class of 12 faculty participated in the year-long fellowship and developed projects that included creating a care transitions mnemonic, new ways to engage pre-nursing students, and a workshop to teach providers how to recognize victims of sex trafficking and use trauma-informed care to help them. Innovation Fellows received pilot funding for each project and additional professional development funds once they completed the program.
“The Innovation Fellowship has helped me grow in the areas of teaching and scholarship,” said inaugural Fellow, Instructor Heather Hyde, DNP, CRNP, CPNP-PC (BSN 2014, MSN 2018, DNP 2020). “Being immersed in the design thinking process gave me the tools to transfer what I have learned into my current manuscripts. Engaging in broader thinking as an educator and constant re-evaluation of my mindset all stemmed from the knowledge I gained from being an Innovation Fellow.”
Developing faculty leadership in health policy is the goal of the Health Policy Fellows, launched in 2023 as part of the UAB School of Nursing Leadership and Health Policy Initiative. This is a two-pronged approach that integrates the School’s recognized excellence in leadership and health policy advocacy to produce a nursing workforce skilled in embedding leadership development and policy change in systems for the future. The initiative helps train faculty, students and community nurses to lead nursing and health care change at all levels, all to build and sustain a strong and diverse cadre of nurse leaders educated to shape equitable and patient-centered health care. Eight faculty made up the inaugural Fellowship that included didactic and experiential learning.

“Participating in the Health Policy Fellows has expanded my view of tangible ways I can make a difference in the future of nursing and in health care outcomes. It also has encouraged me to step outside my comfort zone to engage in opportunities that have potential for sustainable impact that can elevate our profession, influence positive outcomes for patients and their communities on a much greater scale and showing our current and future colleagues how to do the same,” said inaugural Fellow, Associate Professor Melanie Gibbons Hallman, DNP, CRNP, FNP-BC, ACNP-BC, ENP-C, CNS, FAEN, FAAN (BSN 1983, MSN 1990, MSN 1995, DNP 2012).
The allocation of resources to support faculty development also has been a key factor in faculty growth, particularly around scholarship, leading to an increase in papers presented at conferences, publications and national leadership roles in various organizations, said University Professor and Senior Associate Dean for Academic Affairs Linda Moneyham, PhD, RN, FAAN. This includes everything from providing travel funds for faculty to attend conferences, trainings, workshops and other professional development opportunities to offering a year-long Emerging Leader’s program for early career faculty to support basic leadership skill development.
“We invest heavily in faculty development and continue to see the dividends,” Moneyham added. “Attendance at conferences not only keeps the program leaders informed of what is happening in nursing education at the national level, but also prepares faculty to advance their service to professional organizations by assuming leadership roles within these organizations, which in turn well-positions our School in terms of influence and reputation.”
Building research capacity
The School also is building upon its diversified research funding portfolio and well-developed foundation of funded, nationally and internationally renowned nurse scientists who, in addition to their programs of research, are mentors for other faculty and doctoral students. This cultivation of a supportive environment facilitates and inspires innovative and sustainable scholarship across all missions. From providing internal funding sources to dedicated support for external grant submissions, the School is empowering research excellence and impact alongside UAB’s research vision, Growth with Purpose, and the university’s targeted goal of $1 billion in research expenditures.

The Dean’s Scholar Award is a springboard for future funding opportunities. It provides funding for pilot projects across all three missions supporting UAB’s high-growth research areas, quality improvement and translational science projects to provide preliminary data that can be used to apply for other sources of funding. The program also fosters interdisciplinary partnerships with scientists and clinicians within the school, university, health system and health care community. A total of 25 DSA projects have been funded to date, with five DSA projects focused on teaching innovations. Since 2016, 21 faculty have been funded with DSAs and projects resulting from those have brought more than $6 million in new grants, a nearly $20 return for every DSA dollar provided.
Assistant Professor Shena Gazaway, PhD, RN, said the $23,608 DSA award she received in November 2021 for the project “Developing a Collaborative Community Intervention to Train Chronic Kidney Disease Family Caregivers in providing Decision Support” has led to $946,826 of external funding from the Palliative Care Research Cooperative and a K23 career development award from the National Institute of Diabetes and Digestive and Kidney Diseases.
“In addition, the DSA allowed our team to develop a six-member community advisory board of people who identify as chronic kidney disease patients, caregivers or supporters of these individuals that has been invaluable as they share their perspectives and experiences and collaborate fully on study design and intervention material—including content and focus. They are also help with dissemination efforts,” Gazaway said.
Bachelor of Science in Nursing Honors students also are being developed as nurse scientists. They partner with faculty members on a research topic and then lead their own projects and present at the annual UAB Undergraduate Research Expo. For many, it’s their first time learning about the world of nursing research.
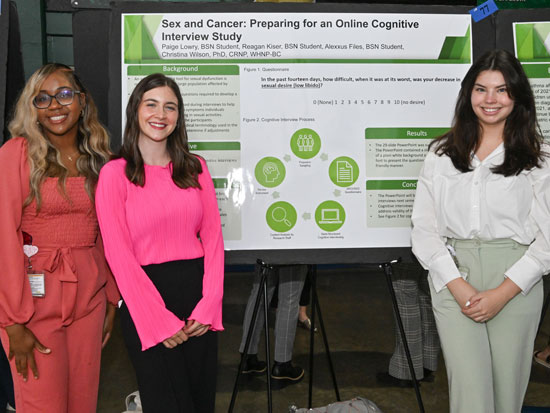
“Being able to do research like this as an undergraduate student has been really amazing because I feel like it’s an experience that not a lot of people get and what I’ve learned, I’ll be able to use as I further my education,” said BSN student Paige Lowry.
The School also is launching new opportunities for nurses in front-line clinical research and building the workforce simultaneously. A graduate certificate in Clinical Research Management is preparing nurses to lead and manage research teams in implementing clinical trials while ensuring compliance with federal regulations for patient safety and ensuring integrity of research findings.
“This is equipping research professionals with the essential skills and knowledge to effectively lead and oversee clinical research studies,” said Associate Professor and Interim Assistant Dean for Graduate Clinical Education – DNP Tedra Smith, DNP, CRNP, CPNP-PC, CNE, CHSE (MSN 2004, DNP 2011). “By understanding the ethical, regulatory and operational aspects of clinical trials, these clinical research professionals can ensure that research is conducted with the highest standards of integrity and patient safety, meaning health care institutions then benefit from improved clinical protocols and innovative treatment strategies.”
Building a resilient nursing workforce
The School’s goals for nursing workforce development also include developing and strengthening of skills and investment in student support, retention strategies and recruitment.
Prior to enrolling as nursing students, first-year undergraduate students take a Nursing 100 course, included in the UAB Freshman Year Experience. This course includes academic skill preparation, orientation to the UAB campus and the profession of nursing, which includes exposure to the School’s advanced simulation technology and nursing skills labs. Students also are offered hands-on experiences through nurse shadowing opportunities, as well as patient transport and food service jobs at UAB Hospital.
Innovative teaching strategies are crucial in an ever-evolving profession, especially in building successful, resilient students at all levels.
Health in the City, taught by Assistant Professor Elizabeth Crooks, DNP, RN, CNE (DNP 2013), is among the university’s Blazer Core electives, and explores how environmental and social determinants contribute to health among those living in urban areas. Emphasis is on policies, planning and strategies used to reduce health disparities and meet the challenges of promoting health in Birmingham and similar mid-sized cities in the United States.
“Students who enroll in this course come from a wide range of backgrounds. Some are the first person in their family to attend college while for others it is the first time they have been away from their rural communities. There are so many different voices in this class. What is common among them, however, is their ability to adapt in the face of stressors, a quality essential to building a resilient nursing workforce. We use Birmingham as the classroom, exploring how the city addresses complex problems that impact health and shows the possibilities nursing holds as a career and the importance of having a nursing workforce that understands and reflects the demographics of the community it serves,” Crooks said.

In 2022, Assistant Professor and Director of Student Retention Jennie Alspach, DNP, RN, FNP-BC (BSN 1996, MSN 1999, DNP 2020), Instructor Rachael Bruce, MSN, MPH, CRNP, FNP-C, CNE (MSN 2016), Instructor Jessica Bumpus, PhD, and Instructor Laketa Huddleston-Pettiway, PhD, M.Ed, developed the Student Success Champions initiative, which aids pre-licensure students on the front-end of academic challenges before they become barriers to successfully completing the nursing program. They also have collaborated with faculty in Nursing 100, Student Success in Nursing and Vulcan Materials Academic Success Center, the University’s academic success center for undergraduates to create med-math modules to help students develop medication dosage calculation skills and encourage participation in VMASC tutoring and supplemental instruction sessions. They also provide networking opportunities with nursing faculty and currently enrolled students to introduce them to the nursing field early on to help foster a sense of community, which is crucial for student success.
“Since the onset of the program, course pass rates have improved, and attrition, especially among underrepresented minority students, has reduced significantly,” Alspach said. “BSN attrition decreased from 22 percent in the 2020-2021 academic year to just 2 percent in the 2022-2023 academic year, enhancing student outcomes and putting more BSN-prepared nurses into the workforce.”
Skills Lab Educator Samantha Berrien, MSN, RN, is piloting the Successful Outcomes of Students in Nursing program she developed to identify learning gaps in skills mastery for individual prelicensure students and provide personalized coaching sessions. It gives nursing students additional help and resources to help ensure success. Berrien tailors her teaching style to the learning style of each student to help them perfect and practice their skills. The strategy has resulted in more confident students and successful skills validations.
This program also supports students who may face challenges outside the classroom, such as those who must work while in school or who are caring for children by providing individual and group mentoring and academic coaching. Throughout the semester, personalized strategies and SMART goals are created to help students work through challenges to achieve success. Students have individual or small group coaching sessions to practice clinical skills and receive real-time feedback on improvements needed before testing. And weekly check-ins are conducted to monitor progress and provide motivation.
Berrien anticipates that through the program, student confidence will increase and exam grades will markedly improve, ultimately leading to better patient care and more confident and competent nurses entering the workforce.
Retention and success strategies also are being implemented in graduate programs.
Assistant Professor Hiboombe Haamankuli, DNP, CRNP, ACNP-BC (MSN 2010), Assistant Professor Sabrina Kopf, DNP, CRNP, ACNP-BC (BSN 2009, DNP 2017), and Assistant Professor Somali Nguyen, DNP, CRNP, AGACNP-BC (BSN 2010, MSN 2014, DNP 2019), are using gamification to teach critical skills such as antimicrobial selection, chest X-ray interpretation and point-of-care ultrasound to improve engagement and knowledge retention among graduate students, ensuring they are well-prepared to excel in clinical practice and deliver high-quality patient care.
The School’s Nurse Anesthesia Pathway recently implemented the WellPro Path, a wellness and professional development plan for incoming students. The plan supports and sets students up for success prior to starting the program and helps ensure all have access to the same resources provided by faculty and current students. Resources range from being academic-focused, including learning and test-taking strategies, to also covering areas of wellness and community, involving support groups and a mentorship program between upperclassmen and new students.
“We’ve seen students with the same recurring stressors and have prospective and incoming students ask us what they can do before beginning the program. The Nurse Anesthesia faculty put together our years of experience and what we’ve observed to create something meaningful to share with students,” said Assistant Professor Katie Woodfin, DNP, CRNA, CHSE (MSN 2014, DNP 2022).
“Our faculty have worked diligently to achieve excellence in teaching by developing innovative teaching strategies that are effective in supporting students achieve mastery of knowledge and skills required for excellence in nursing practice, helping create a resilient nursing workforce,” said Moneyham said.
Integrating interprofessional simulation and practice experiences
Interprofessional education is an important strategy the School uses to better prepare students for practice. Partnering with the UAB Office of Interprofessional Curriculum, interprofessional team training led by trained faculty facilitators provides opportunities for prelicensure and graduate students to learn and practice essential skills for effective functioning in future interprofessional teams.

Students work together to assess a patient’s needs and create an individualized care plan. Teams consist of students from up to 12 different professions. IPTT is a 90-minute activity regularly held in the spring, summer and fall semesters. Nearly 7,000 students from nursing, medicine, dentistry, nutrition, social work, physical therapy, occupational therapy, public health, respiratory therapy, physician assistant, optometry, pharmacy and clinical lab sciences have participated in IPTT since 2016.
“It is critically important that our graduates are practice-ready for interprofessional models of care,” said Professor, Chair of the Acute, Chronic and Continuing Care Department and Director of the Office of Interprofessional Curriculum Allison Shorten, PhD, RN, FACM, FNAP, FAAN. “We know that patients and families in our community are more likely to experience health improvement when they are supported by high functioning interprofessional health care teams. Graduates of our nursing programs are educated to appreciate the power of teamwork, be confident in their ability to communicate and collaborate with others and serve as role models and leaders in interprofessional practice.”
A valuable complement to this classroom learning is real-world experience for undergraduate and graduate students afforded by the School’s active faculty practices and nurse-managed interprofessional collaborative practices.
Through team-based care in the School’s nurse-managed clinics, PATH (Providing Access to Healthcare) and HRTSA (Heart FailuRe Transitional Care Services for Adults), which are part of the UAB Nursing Partnership, an academic-practice partnership of the UAB School of Nursing and UAB Health System, faculty provide clinical preparation for both undergraduate and graduate students from a variety of disciplines. Both use the interprofessional collaborative practice model, STAND-UP (Smooth Care Transitions for Diverse and Underserved Populations) to integrate interprofessional education and collaborative practice for chronic disease management of vulnerable populations.
PATH provides diabetes care to an uninsured, medically underserved population discharged from UAB Hospital. HRTSA provides heart failure care to the same patient base. Their services include guideline-directed care from nurse practitioner visits, physician visits, optometry, nutrition, mental health, physical therapy, behavioral health and assistance in obtaining needed medications and/or testing supplies at the lowest possible cost, as well as education for patients and their caregivers.
“Implementing interprofessional collaborative practice models allows students to practice and improve their skills and be an important part of a care team while still learning in the classroom,” said Professor and Associate Dean for Clinical and Global Partnerships Michele Talley, PhD, CRNP, ACNP-BC, FAANP, FAAN, FNAP (MSN 2005, PhD 2015). “The team-based approach also optimizes the distinct contributions of various disciplines, resulting in improved patient care.”
The School is also working to improve mental health access across Alabama and increase the behavioral health workforce through a partnership with Bibb Medical Center. Psychiatric-mental health nurse practitioner students and medical residents receive hands-on experience and training as part of interprofessional teams, integrated behavioral health, trauma-informed care, telehealth and resilience while they address the needs of patients across the lifespan.
Coinciding with interprofessional education and practice, simulation and emerging technologies are at the forefront of the School’s teaching strategies.
The School is a recognized leader in innovative and engaging simulation experiences. In June 2024, members of the Office of Technology and Innovation received the Frontline Simulation Champion Excellence Award from the International Nursing Association of Clinical Simulation and Learning. The team was recognized for going beyond the ordinary dedication to excellence in the delivery of simulation-based learning, creating realistic and immersive scenarios that closely mirror real-life clinical situations. Simulations include dynamic pre-briefing experiences to ensure student readiness to learn, simulation experiences within an environment of psychological safety and a robust debriefing program based on best practices.
“Simulation has significant value and impact on students and their learning experience, and we are fortunate that our administration supports this important work,” said Professor and Associate Dean for Technology and Innovation Penni Watts, PhD, RN, CHSE-A, FNAP, ANEF, FSSH, FAAN (PhD 2015). “The simulation team consistently goes above and beyond, ensuring that simulation activities are realistic, engaging and aligned with the learning objectives. Their attention to detail and dependability have fostered an environment of trust and professionalism, where students feel supported and empowered to learn and grow.”
Enhancing access, engagement and well-being
Nursing education and workforce development extend beyond current nursing students. Through a partnership with Birmingham City Schools, the School reaches middle school and high school students to expose them to the nursing profession.
Led by Professor and Associate Dean for Access and Engagement Felesia Bowen, PhD, DNP, PPCNP-BC, FADLN, FAAN, the Pathway to Professional Nursing, which launched in fall 2023, is for high school students and designed to prepare students for college and a career in nursing.
While in high school, students learn about the different areas of nursing and nursing skills, take advanced and dual-enrollment classes, visit the UAB campus and participate in summer enrichment activities. They also gain research and quality improvement experience working with UAB nurse scientists on scholarly projects. The program also provides students with an opportunity to become certified as patient care technicians after graduating from high school, providing them a path to employment if they choose not to immediately attend college. Since the program’s launch, 43 students have been admitted.
While in high school, students learn about the different areas of nursing and nursing skills, take advanced and dual-enrollment classes, visit the UAB campus and participate in summer enrichment activities. They also gain research and quality improvement experience working with UAB nurse scientists on scholarly projects. The program also provides students with an opportunity to become certified as patient care technicians after graduating from high school, providing them a path to employment if they choose not to immediately attend college. Since the program’s launch, 43 students have been admitted.
“We are very proud of our scholars in the Pathway to Professional Nursing program. Over the summer, eight students from the inaugural cohort traveled to Texas to participate in the HOSA (Health Occupations Students of America) Future Health Professionals competition,” Bowen said. “Our goal is to continue to build the number of students in each cohort as we obtain resources to support program expansion.”
The School’s Booker T. Washington K8 Health Club began in 2022 as part of a $250,000 Health Resources and Services Administration grant to promote positive health behaviors in children and their families, and to develop the future nursing workforce. Working with seventh and eighth grade students who are interested in a potential health care career, they are taught good health habits and exercise, as well as about the nursing profession. They also come to the School to tour simulation spaces, shadow nursing students in the skills lab and complete a babysitting simulation case in the School’s home health simulation suite.

Supporting the current nursing workforce, including UAB School of Nursing faculty, staff, students and alumni, also is a priority for access and engagement. The Health Resources and Services Administration awarded Professor and Rachel Z. Booth Endowed Chair in Nursing Patricia A. Patrician, PhD, RN, FAAN, a three-year, $2.3 million Health Workforce Resiliency Award to implement and study programs to reduce burnout and promote mental health and well-being within the nursing profession in collaboration with UAB Medicine.
In its first year, WE CARE provided nursing professional development specialists trained in resilience and psychological first aid, and a nurse wellness manager to provide individualized support services exclusively to nurses at UAB Medicine. During the second year of the grant, efforts were turned toward the School, creating a Wellness Room, bringing on a psychiatric-mental health nurse practitioner and a social worker for students, faculty and staff to provide support and help them learn to manage stress and respond compassionately to others in distress. Wellness modules also were created for students that focused on diet, exercise, sleep, mental health, stress and resilience. Now in its third year, the program’s focus has been on interventions throughout the state, particularly working with hospitals in rural areas.
“Nurses are the backbone of the health care system and need resources that help them during tumultuous times to support their mental well-being,” Patrician said. “The work we continue to do not only meets the needs of nurses, it also helps Alabama’s families by improving access to high-quality and safe patient care through a resilient nursing workforce.”
Building practice capacity
Clinical partners who provide students employment opportunities while in school utilize the skills they are learning to help provide support in the clinical environment. In turn this provides students real-world experiences in health care to help ease their transition to the professional nursing role and help them earn money while in school.
The Student Nurse Intern Program, a partnership between the School and Children’s of Alabama, allows nursing students an opportunity to work in a clinical extender position providing valuable on-the-job experience. Clinical Extenders are paired with a bedside nurse helping them gain insight into communication and interactions between nurses and caregivers, patients and other members of the multidisciplinary team. The results are competent, confident members of the health care team with firsthand knowledge of teamwork and other useful skills.
“This opportunity benefits the students and the hospital. It helps them transition into the role of a pediatric nurse with more confidence and knowledge of the policies and procedures within Children’s,” Smith said. “This includes foundational knowledge of the electronic health record which causes a lot of anxiety for new nurses.”

The UAB Nursing Partnership with UAB Medicine offers positions as nursing student graduate aides and patient care technicians, and the Birmingham VA Medical Center offers student nurse technician and graduate nurse technician positions.
“Through our unique partnership, we can offer opportunities for students in addition to the traditional clinical rotations," said UAB Hospital Chief Nursing Officer Terri Poe, DNP, RN, NE-BC (BSN 1986, DNP 2013). “The Nursing Student Graduate Aid role was inspired by the partnership during the COVID-19 pandemic and remains a valuable role on the nursing units, allowing students to serve on interprofessional care teams to assist with patient care. Students also assist with vital signs, transportation, and providing the activities of daily living for patients when they are employed in the new Patient Care Technician role. Both of these positions provide much needed support on the nursing units as well as preparation for the students who will soon enter the nursing workforce.”
The school also provides students opportunities to impact and contribute to nursing practice before they enter the workforce.
Nurse educator graduate students are working with mental health faculty and nurse practitioners at the School of Nursing to develop educational modules that assist UAB Hospital staff nurses to navigate and de-escalate challenging behavioral health situations in the clinical environment. The modules are associated with eight behavioral health conditions and developed into a series of PowerPoint presentations that will be hosted on an available nursing-centric website. The goal of this education for practitioners is to provide direction to the staff nurse for better understanding their patients and integrating care delivery interventions specific to their behavioral health needs. These educational resources work to enhance staff nurses' confidence and competence when addressing behavioral health crises. Through this initiative, frontline nurses will be better equipped to deliver comprehensive and compassionate care for patients with both medical and behavioral health needs.
Boldy blazing forward, elevating excellence to new heights
The School’s new strategic plan provides a strong foundation for setting the School up to continue its legacy of success with a shared vision and mission in mind. Through forward thinking approaches and individual and collective contributions, the School will address changes and trends in the ever-evolving areas of nursing education, higher education, nursing practice and the broader health care industry, to produce leaders who transform health in a dynamic society.
“We are proud of our focused strategic plan built over the last 18 months with the input and energy of our various stakeholders,” Shirey said. “Our plan was vetted and ratified by our School of Nursing shared governance structure inclusive of our Faculty Organization and Staff Council. It is well-aligned with the broader University's strategic plan.”