UAB nursing school to study palliative care for vets, minorities, rural cancer patients
The University of Alabama at Birmingham (UAB) School of Nursing has received a four-year, $720,000 grant from the American Cancer Society to study whether a phone-based palliative care intervention can help reduce access disparities for veterans, minorities and patients from rural areas who have advanced cancer.
 Palliative care focuses on providing patients with relief from the symptoms, pain and stress of illness. Research shows that when patients with incurable cancer receive palliative care along with regular cancer treatment, they have a better quality of life, as well as less symptoms and depression, and they may live longer.
Palliative care focuses on providing patients with relief from the symptoms, pain and stress of illness. Research shows that when patients with incurable cancer receive palliative care along with regular cancer treatment, they have a better quality of life, as well as less symptoms and depression, and they may live longer.Over the past decade, the study’s principal investigator, Marie A. Bakitas, D.N.Sc., APRN, FAAN, professor of nursing and Marie L. O'Koren Endowed Chair, has worked to develop Project ENABLE (Educate, Nurture, Advise, Before Life Ends), a phone-based palliative care intervention for patients. Initial work has been done in an academic medical center setting.
“Nearly 60 million Americans, many of them veterans and ethnic minorities, live in rural areas where few palliative care services exist,” Bakitas said. “The American Cancer Society has set a nationwide objective to eliminate cancer disparities by 2015. Given that advanced cancer patients in rural areas are less likely to benefit from palliative services due to limited access and suboptimal care, we believe this intervention will provide an innovative way for cancer centers in these areas to provide palliative care.”
In the original ENABLE II study, a specially trained advanced practice nurse coached patients and their caregivers through a series of structured telephone sessions on topics such as problem solving, communication, symptom management and self-care, as well as medical decision-making. The participants had four weekly educational sessions and monthly follow-up sessions.
| Research shows that when patients with incurable cancer receive palliative care along with regular cancer treatment, they have a better quality of life, as well as less symptoms and depression, and they may live longer. |
“The patients who underwent this intervention had a better quality of life, less depression and lived longer than patients who received only regular cancer care,” Bakitas said. “This is extending the results of that study to patients and family members in the community.”
Bakitas said the project will target four communities representing rural geography and/or ethnic and racial diversity: Birmingham, Ala. (Birmingham VA Medical Center); Grand Rapids, Mich.; Spartanburg, SC.; and Bangor, Maine. Project teams at each site will work together over the next four years to tailor ENABLE to their individual communities.
“Our short-term goal is to learn the best way to bring palliative care services to patients and families to improve care and quality of life, as well as reduce the burden of cancer in these four communities,” Bakitas said. “We also will develop a toolkit that can be used to implement the model.”
The project’s long-term goal, Bakitas added, is to make this project accessible to patients and family members in other non-academic community cancer centers across the country.
“In so doing, we hope to reduce the suffering of patients living with cancer nationwide,” she said.
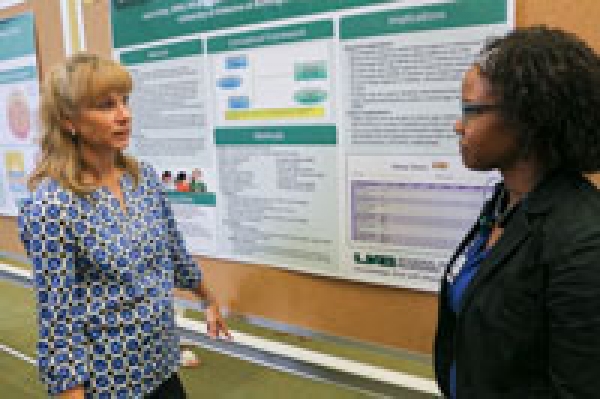
May 13-17, 2013, is National VA Research Week. On May 15, Bakitas is discussing a related project involving veterans during a poster presentation at the Birmingham VA Medical Center. The poster, “Oncology Clinicians’ Perspectives on Providing Palliative Care for Patients with Advanced Cancer,” was built upon data collected from her palliative care research at White River Junction VA Medical Center in Vermont.