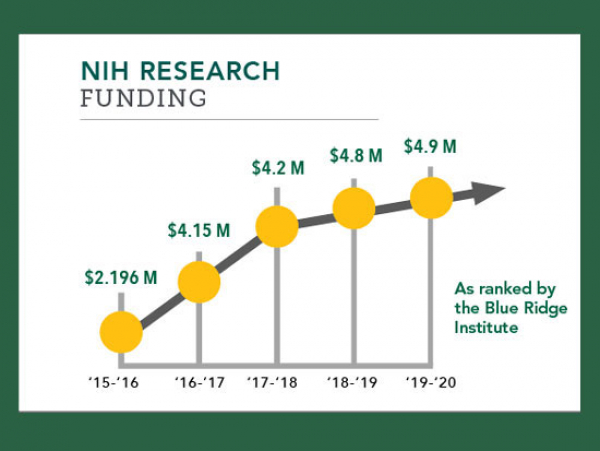
University of Alabama at Birmingham (UAB) School of Nursing Professor and Marie L. O’Koren Endowed Chair Marie Bakitas, DNSc, NP-C, FAAN, has received a five-year, $3.5 million R01 grant from the National Institute of Nursing Research (NINR), a part of the National Institutes of Health (NIH), for a study to determine whether palliative care provided when advanced heart failure patients are still well will result in better quality of life, mood, and less symptom distress/burden, for patients and/or caregiver, when compared to usual heart failure care.
 This randomized controlled trial, “ENABLE: CHF-PC (Comprehensive Heartcare for Patients and Caregivers),” will compare the quality of life, symptom burden, mood, and the quality of life in 380 older adults with stage III/IV heart failure and their family caregivers. Half of the patient participants will be randomized to the intervention and half will receive usual heart failure care.
This randomized controlled trial, “ENABLE: CHF-PC (Comprehensive Heartcare for Patients and Caregivers),” will compare the quality of life, symptom burden, mood, and the quality of life in 380 older adults with stage III/IV heart failure and their family caregivers. Half of the patient participants will be randomized to the intervention and half will receive usual heart failure care.
“Despite treatment advances, 50 percent of heart failure patients will die within five years,” said Bakitas, who also is Associate Director of the UAB Center for Palliative and Supportive Care. “Increasing age and rural environment are risk factors associated with the greatest heart failure complications and death. And, in the year before death, research shows heart failure patients will experience multiple hospitalizations and personal and economic costs of unrelieved physical and emotional suffering. The overall goal of this study is to test the efficacy of a heart failure palliative care telehealth model in reducing the suffering and burden from symptoms associated with living with advanced heart failure.”
Palliative care, she said, has been demonstrated in other diseases to reduce end-of-life suffering, hospital readmissions, and health care costs, but only 16 percent of Alabama hospitals have palliative care programs compared with the national average of 53 percent.
Bakitas added that of Alabama’s 67 counties, 55 are categorized as rural and the incidence of heart failure in these rural counties is greater than that of the state’s urban counties, making an intervention such as this key to improving quality of life for rural Alabama residents with heart failure and their families.
“There is an urgent need to increase palliative care access to older adults with advanced illness, especially in the south which has the lowest availability to these services,” she said. “It is critical to understand how to best make this care accessible to this population.”
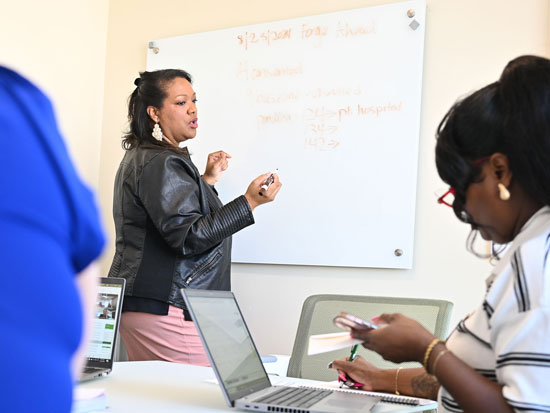
The focus of this palliative care model is on coaching patients and their family caregivers in problem-solving, communication, symptom management, and health care decision-making with a goal of empowering them to be better prepared to meet the challenges of progressive illness, Bakitas said. This is a telehealth intervention, meaning patients and their caregivers do not have to leave home to participate after a single in-person palliative care assessment. The in-person consultation is followed by a series of phone sessions for a period of 48 weeks, specifically tailored to meet the needs of a rural population.
Bakitas and others have demonstrated in advanced cancer that concurrent palliative care offered from the time of advanced diagnosis achieves beneficial quality of life, symptom burden, depression, and in some cases survival outcomes. The intervention in this study is adapted from Bakitas’ successful palliative care model for cancer (ENABLE: Educate, Nurture, Advise, Before-Life-Ends).
Advanced heart failure affects nearly six million Americans, and less is known about how this illness affects the 80 percent of heart failure patients who are 65 years and older because research tends to focus on younger patients. Currently, Bakitas said, only 19 percent of Medicare-aged heart failure patients and their family caregivers access palliative care services, compared with more than half of advanced cancer patients.
“Older patients with heart failure and their family caregivers, rarely have access to palliative supportive care services because the disease is unpredictable and in the current health care system, palliative treatment may not be provided until after other medical treatments have been tried,” Bakitas said.
Also important to the study is the impact that palliative care has on caregiver burden. This study will examine the impact of the intervention on caregivers’ self-reported quality of life, mood, health and caregiving burden.
“This is important because caregivers can spend an average of eight hours each day assisting the patient with their care,” she said. “This takes a toll on their physical and psychological well being. Caregivers will often ignore their own needs and ultimately without assistance that this coaching is designed to provide, caregiving studies have documented that they can have higher rates of illness and death.”