By Erica Techo
Everyone experiences stress in their daily lives. Children and families of color can experience even higher levels due to preexisting factors like poor social determinants of health and transgenerational stressors. In health care, nurse practitioners have a unique opportunity to assess and identify these stressors in order to help promote improved health outcomes.
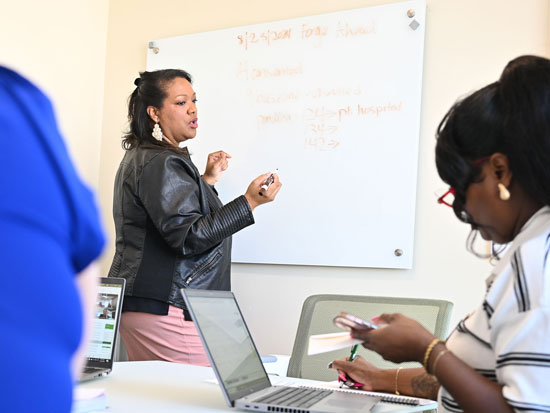
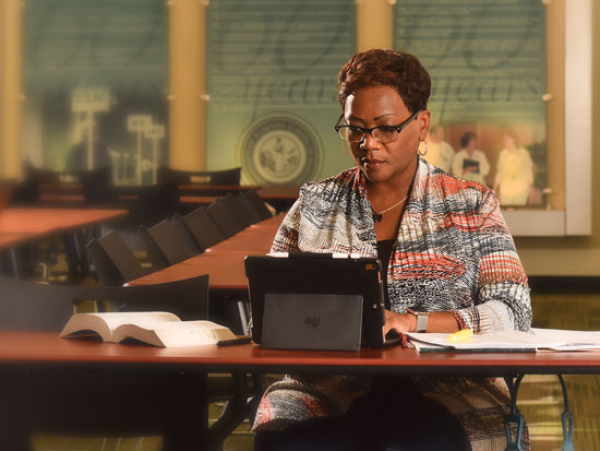
One framework that describes compounding stressors and their impact on children is the Toxic Stress Schema, recently introduced in a paper by University of Alabama at Birmingham School of Nursing professor and Associate Dean of Diversity, Equity and Inclusion Felesia Bowen, PhD, DNP, APRN, PPCNP-BC, FAAN.
The article, titled, “A Schema of Toxic Stress Informed by Racism, Transgenerational Stress, and Disadvantage,” was published in the Journal of Pediatric Health Care in October 2021 and uses the COVID-19 pandemic as an example of the “stress storm” that exists within the toxic stress schema.
“What we say in this paper is that, as health care providers, when we encounter children, we must understand that they are exposed to stressors all the time,” Bowen said. “The adults in their lives offer protective factors and buffer those stressors, which means the children experience lower levels of stress. But when the stress is not buffered, or an event occurs that weakens those protective factors, that can lead to toxic stress.”
When considering stressors and the central event, it is also important to look at advantage. The toxic stress schema includes a spectrum of advantage, where on one end higher advantage means more protective factors. On the other end of the spectrum, a lack of advantages can lead to major gaps in protection thus increasing the negative effects of stress.
“Families can fall anywhere on the continuum of advantage. Their place is not static, they can also move up and down depending on their circumstances,” Bowen said. “For example, a family might have a steady source of income, stable housing, and food—but then the pandemic takes place, and a parent loses their job, they have difficulty paying rent/mortgage and purchasing food to last through the month.”
Each of these factors can impact, and oftentimes weaken, protective factors that shield a child from toxic levels of stress, especially when their parents are stressed and unable to buffer for them. Toxic stress has both physical and mental repercussions for the child, Bowen said, and it is important to understand how prolonged exposure to stress can lead to long-term, negative health effects.
It is also important to remember, Bowen said, that children and families of color already experience higher levels of stressors due to structural racism, discrimination, generational trauma and more. These factors are represented within the toxic stress schema, which illustrates how these can negatively impact a family’s protective factors.
“We advise nurse practitioners to consider these things. We need to assess for these stressors when we’re talking with families, and we need to also consider social determinants of health and adverse childhood experiences,” Bowen said.
To assess a child’s toxic levels of stress, Bowen and her coauthors crafted questions that correspond to social determinants of health and diagnoses that can be officially coded. This provides nurse practitioners with a next step in order to catch potential challenges and stressors.
“Every visit, every encounter needs to include these assessments because families move along the advantage spectrum. Consistency in assessing can lead to early intervention, which can strengthen those protective factors and move them to the left on the spectrum, closer to advantages versus disadvantages,” Bowen said.
The article is available to view at this link.